Sepsis and Septicemia are distinct yet interconnected conditions involving systemic inflammation and infection, with septicemia specifically referring to the presence of microorganisms in the bloodstream.
Definition of Sepsis
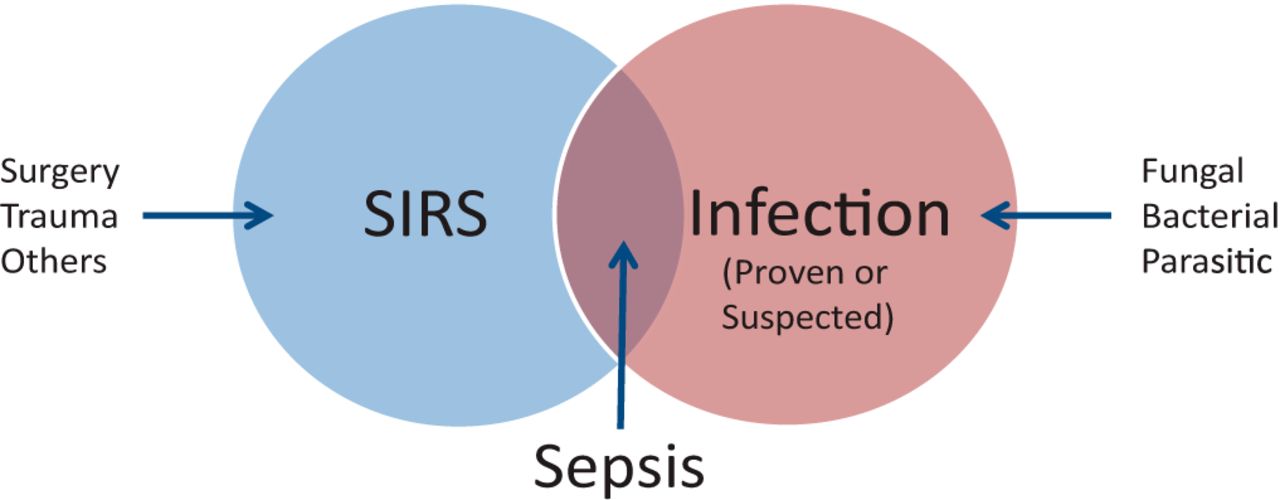
Sepsis is a life-threatening medical emergency resulting from improper immune system responses to infections that become dysregulated, inciting widespread inflammation across multiple organs and systems in the body and creating systemic inflammatory response syndrome (SIRS). Sepsis requires prompt medical intervention in order to minimize further complications or risk and potential mortality.
Definition of Septicemia
Septicemia (also referred to as bloodstream infection or bacteremia) is a severe infection in which pathogens, including bacteria, enter and multiply within the bloodstream. Septicemia may result from pneumonia, urinary tract infections, skin infections or abdominal infections and is marked by pathogen presence which triggers systemic inflammation that leads to organ dysfunction as well as potentially life-threatening complications requiring immediate diagnosis and treatment in order to limit further progression into sepsis and decrease mortality risk.

Importance of understanding the difference between Sepsis and Septicemia
Understanding the difference between Sepsis and Septicemia is crucial for several reasons:
- Accurate diagnosis and treatment of Sepsis and Septicemia: Differentiating between Sepsis and Septicemia allows healthcare professionals to accurately diagnose the conditions, as well as provide appropriate treatments. Although management strategies for sepsis and septicemia may differ depending on its cause; misdiagnosis could delay initiating necessary interventions and jeopardize patient outcomes.
- Clinical decision-making of Sepsis and Septicemia: Recognizing the distinction between sepsis and septicemia enables healthcare providers to make informed clinical decisions. Understanding the specific characteristics and manifestations of each condition helps guide the selection of appropriate diagnostic tests, treatment options, and monitoring parameters.
- Prognostic implications of Sepsis and Septicemia: The differentiation between sepsis and septicemia can have prognostic implications. Sepsis, which involves a dysregulated immune response and organ dysfunction, carries a higher risk of morbidity and mortality compared to septicemia. Understanding the severity and potential outcomes of each condition allows healthcare providers to assess the patient’s prognosis and make appropriate care plans.
- Epidemiological and research purposes of Sepsis and Septicemia: Distinguishing sepsis from septicemia is vitally important for accurate epidemiological data collection and research studies, providing greater insights into incidence, prevalence and risk factors associated with each condition – leading to improved public health interventions and clinical practices.
- Patient and public awareness of Sepsis and Septicemia: Education of the general public on the differences between sepsis and septicemia can increase awareness about both conditions. Acquiring more knowledge can enable early recognition of symptoms, prompt medical assistance and better outcomes for individuals at risk of sepsis or septicemia.
Understanding the differences between Sepsis and Septicemia are vitally important to healthcare providers, researchers, and the general public in order to provide optimal patient care, implement targeted interventions, and reduce the impact of serious infections like these.
Sepsis
Sepsis is a life-threatening medical emergency caused when your immune response to an infection becomes out-of-control and leads to widespread inflammation in your body.
Immediate medical intervention must take place – here are a few key points about sepsis:
- Infection: Sepsis typically arises as the result of an infection caused by bacteria, viruses, fungi or parasites and can occur anywhere from within a host body such as their lungs, urinary tract, abdomen or skin.
- Immune response: As soon as our bodies detect infections, the immune system responds immediately. But in sepsis, this response becomes disregulated and excessive resulting in widespread inflammation throughout our entire bodies.
- Systemic inflammatory response syndrome (SIRS): Sepsis is defined by systemic inflammatory response syndrome (SIRS), an abnormal immune reaction which impacts multiple organ systems simultaneously. Common indicators of SIRS may include increased heart rate and respiratory rate as well as abnormal body temperatures such as fever or hypothermia as well as an unusual white blood cell count.
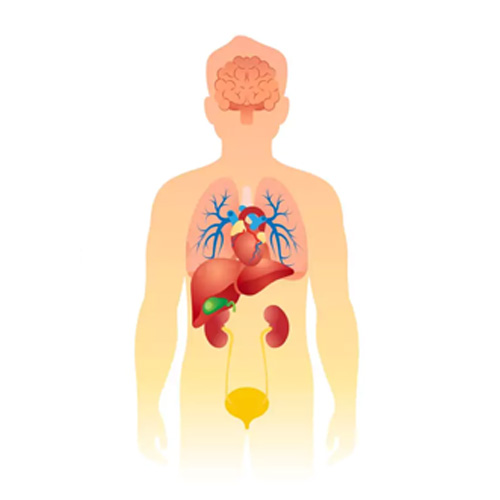
- Organ dysfunction: As sepsis progresses, it can cause organ dysfunction or failure – particularly of lungs, kidneys, liver, heart and brain – leading to severe complications or even fatality if treated quickly and correctly.
- Severity classification: Sepsis can be classified into different stages based on the severity of the condition. The Sequential Organ Failure Assessment (SOFA) score and the quick SOFA (qSOFA) criteria are commonly used to assess the severity and predict the risk of mortality in sepsis.
- Symptoms: Sepsis symptoms vary; however, typically include fever, chills, rapid breathing, increased heart rate and decreased blood pressure as well as confusion or disorientation with decreased urine output and skin rash or discoloration.
- Diagnosis: Sepsis can be diagnosed through clinical evaluation, physical exam and laboratory tests such as blood cultures or imaging studies to pinpoint its source and assess severity.
- Treatment: Prompt treatment is essential in sepsis to prevent its progression and improve outcomes. Treatment typically involves administration of antibiotics to target the infection, intravenous fluids to maintain blood pressure, and other supportive measures to stabilize vital signs and organ function. In severe cases, intensive care management may be necessary.
- Long-term effects: Post-sepsis syndrome affects survivors of sepsis in long-term ways that include physical, psychological and cognitive effects that include muscle weakness, fatigue, memory problems anxiety or depression requiring rehabilitation and support services in recovery stages. Rehabilitation may also be required during this period to aid their full recovery process.
- Prevention: Preventing infections and promptly treating any suspected infections can help reduce the risk of developing sepsis. Vaccinations, proper wound care, and adherence to infection control measures in healthcare settings are important preventive measures.
Sepsis is an urgent medical condition requiring immediate medical treatment, so knowing its signs and symptoms, seeking timely medical care and raising awareness are vital in saving lives and improving outcomes of those afflicted by sepsis.
Septicemia
Septicemia (also referred to as bloodstream infection or bacteremia) is an acute medical condition characterized by the presence and multiplication of microorganisms like bacteria in your bloodstream.
Here are a few key points about it:
- Infection in the bloodstream: Septicemia occurs when bacteria or other pathogens enter the bloodstream and spread throughout the body. The bloodstream serves as a pathway for the bacteria to reach various organs and tissues.
- Source of infection: Septicemia may result from various sources, including lung (pneumonia), urinary tract or cellulitis infections; abdominal infections like appendicitis or peritonitis; medical devices (such as catheters); or infections related to medical devices.
- Bacterial dissemination: Septicemia-causing bacteria enter the bloodstream through any breach in its natural defenses – from wounds or surgical sites, or through infected organs. Once inside, however, they quickly multiply and spread throughout the body.
- Systemic inflammatory response: Pathogens entering the bloodstream cause a systemic inflammatory reaction from which your immune system releases anti-infective mediators to combat it; however, an excessive or unchecked response could result in widespread inflammation that threatens organ damage.
- Symptoms and clinical presentation: Septicemia symptoms may include fever, chills, rapid breathing, increased heart rate and low blood pressure resulting in confusion or skin rash; its severity will depend on both its source and an individual’s immune response to infection.
- Diagnosis: Diagnosing Septicemia Requires Blood Cultures Blood cultures may be performed to identify bacteria or pathogens present in the bloodstream; additional laboratory tests may also be administered to assess severity and organ functionality of any infection present.
- Complications and outcomes: Untreated or inadequately treated septicemia can result in severe complications, including sepsis, septic shock, organ failure and even death. Early recognition and prompt treatment are vitally important to improve outcomes and ensure survival rates remain positive.
- Treatment: Septicemia requires hospitalization, administration of antibiotics that target specific bacteria responsible, supportive care to stabilize vital signs and organ functions and intensive care management in extreme cases.
- Prevention: Preventative measures against septicemia include proper wound care and infection control protocols in healthcare settings; proper use and maintenance of medical devices; as well as prompt treatment of infections to stop their spread to bloodstream.
- Prognosis: Prognosis for septicemia depends upon various factors, including its source, severity of condition, treatment timeliness and overall health of an individual. Early recognition, appropriate antibiotic treatment regimen and immediate supportive care services all play a part in improving outcomes for treatment of this illness.
Septicemia is a serious condition that requires immediate medical attention. Early detection, appropriate treatment, and preventive measures can help reduce the risk of complications and improve outcomes for individuals with septicemia.
Key Differences Between Sepsis and Septicemia
There are several key differences between Sepsis and Septicemia.
- Definition and Focus:
- Sepsis: Sepsis is a life-threatening condition characterized by a dysregulated systemic inflammatory response to infection, which can lead to organ dysfunction and failure.
- Septicemia: Septicemia specifically refers to the presence and multiplication of microorganisms, such as bacteria, in the bloodstream.
- Scope of Infection:
- Sepsis: Sepsis encompasses a broader concept and includes the body’s systemic response to infection, irrespective of the source or location.
- Septicemia: Septicemia is limited to the bloodstream, where the microorganisms are circulating and multiplying.
- Inflammatory Response:
- Sepsis: Sepsis involves a dysregulated and exaggerated inflammatory response throughout the body, leading to widespread inflammation and organ dysfunction.
- Septicemia: Septicemia triggers a systemic inflammatory response, but the focus is primarily on the bloodstream where the infection is present.
- Diagnostic Criteria:
- Sepsis: The diagnosis of sepsis is based on clinical criteria that include evidence of infection along with the presence of systemic inflammatory response syndrome (SIRS) and organ dysfunction.
- Septicemia: Diagnosis of septicemia involves the identification of microorganisms in the bloodstream through blood cultures or other diagnostic tests.
- Clinical Presentation:
- Sepsis: Sepsis typically presents with multiple systemic symptoms, including fever, rapid heart rate, elevated respiratory rate and low blood pressure accompanied by signs of organ dysfunction.
- Septicemia: Septicemia symptoms may include fever, chills, rapid breathing, increased heart rate and signs of infection – with bloodstream issues as the focus.
- Relationship:
- Sepsis: Sepsis can occur as a progression from an initial infection, including septicemia, but it extends beyond the presence of microorganisms in the bloodstream.
- Septicemia: Septicemia is an infection in which microorganisms enter your bloodstream, potentially leading to sepsis and increasing its severity.
- Treatment Approach:
- Sepsis: Treatment of sepsis involves addressing the underlying infection, providing supportive care, and managing organ dysfunction and complications.
- Septicemia: Treatment of septicemia focuses on eradicating the microorganisms from the bloodstream using appropriate antibiotics and managing any associated complications.
Understanding these distinctions is critical for healthcare providers to accurately diagnose and treat patients, while researchers and public health officials need to gather accurate data in order to develop suitable prevention and treatment plans.
Comparison chart
Comparison chart between Sepsis and Septicemia:
| Aspect | Sepsis | Septicemia |
|---|---|---|
| Definition | Life-threatening systemic inflammatory response to infection | Presence and multiplication of microorganisms in the bloodstream |
| Scope | Broad systemic response to infection | Focused on the bloodstream and its implications |
| Inflammatory Response | Dysregulated and exaggerated inflammatory response | Systemic inflammatory response, primarily in the bloodstream |
| Diagnostic Criteria | Clinical criteria, including infection, SIRS, and organ dysfunction | Identification of microorganisms in the bloodstream through blood cultures |
| Clinical Presentation | Systemic symptoms, organ dysfunction | Symptoms of infection, potential signs of bacteremia |
| Relationship | Sepsis can develop from various infections, including septicemia | Septicemia can be a cause of sepsis |
| Treatment Approach | Address underlying infection, supportive care, manage organ dysfunction | Eradicate microorganisms from the bloodstream with antibiotics, manage complications |
| Complications | Septic shock, multiple organ failure | Organ dysfunction, sepsis development |
| Prognosis | Higher risk of morbidity and mortality | Risk of progression to sepsis, outcomes depend on early treatment |
| Prevention | Infection prevention, timely treatment | Infection control measures, proper wound care, prevention of bloodstream infections |
| Importance of Differentiation | Accurate diagnosis, appropriate treatment, improved outcomes | Tailoring treatment plans, understanding infection source and severity |
Similarities between Sepsis and Septicemia
While Sepsis and Septicemia have important differences, there are also some key similarities between the two conditions.
Here are a few of the shared aspects:
- Infection as a trigger: Both sepsis and septicemia are triggered by the presence of an underlying infection. In both cases, microorganisms, such as bacteria, enter the body and can cause a systemic response.
- Inflammatory response: Both sepsis and septicemia involve a systemic inflammatory response. In sepsis, the immune system’s response becomes dysregulated and leads to widespread inflammation, while in septicemia, the presence of microorganisms in the bloodstream triggers a systemic inflammatory response.
- Organ involvement: Both conditions can result in organ dysfunction and failure. The inflammatory response and potential spread of infection can affect multiple organs, such as the lungs, kidneys, liver, heart, and brain.
- Potential complications: Both sepsis and septicemia can lead to severe complications if left untreated or inadequately managed. These complications may include septic shock, acute respiratory distress syndrome (ARDS), multiple organ failure, and even death.
- Importance of early recognition and treatment: Early recognition and prompt treatment are critical for both sepsis and septicemia. Rapid administration of appropriate antibiotics, fluid resuscitation, and supportive care can improve outcomes and reduce the risk of complications.
- Similar risk factors: Many of the risk factors for sepsis and septicemia overlap. These may include advanced age, immunosuppression, chronic medical conditions (such as diabetes or lung disease), recent surgery or invasive procedures, and prolonged hospitalization.
- Need for prevention: Prevention strategies for both sepsis and septicemia emphasize infection prevention and control measures. This includes proper hand hygiene, appropriate use and maintenance of medical devices, timely administration of vaccinations, and infection control protocols in healthcare settings.
While understanding the similarities between sepsis and septicemia is important, it is equally crucial to recognize their differences to ensure accurate diagnosis, appropriate treatment, and optimal patient care.
Conclusion
Sepsis and Septicemia are two distinct but interlinked conditions with important differences. Sepsis refers to an acute systemic immune response to infection characterized by widespread inflammation and organ dysfunction; on the other hand, septicemia refers to microorganisms being present and multiplying within bloodstream systems – understanding these distinctions is vital in order to provide accurate diagnoses, appropriate treatments, and improved patient outcomes.