SLE and Lupus Nephritis is a chronic autoimmune disease characterized by the immune system mistakenly attacking healthy tissues throughout the body. One common and potentially severe manifestation of SLE is Lupus Nephritis, where the kidneys become inflamed, leading to various renal complications. Lupus Nephritis occurs when the immune system targets the kidneys, causing inflammation that can impair their function.
This condition significantly contributes to the morbidity and mortality associated with SLE, highlighting the importance of timely diagnosis and management to preserve renal function and improve overall outcomes for individuals affected by this complex autoimmune disorder.
Definition of SLE
Systemic Lupus Erythematosus (SLE) is a chronic autoimmune disease in which the immune system mistakenly attacks various tissues and organs in the body. This systemic autoimmune disorder can affect multiple systems, including the skin, joints, kidneys, heart, lungs, brain, and blood cells. SLE is characterized by a wide range of symptoms that can vary in severity, such as joint pain, skin rashes, fatigue, and inflammation.

The exact cause of SLE is not fully understood, but it is believed to involve a combination of genetic, environmental, and hormonal factors. Diagnosing SLE can be challenging due to its diverse symptoms, and treatment typically involves managing symptoms and preventing flare-ups through medications and lifestyle adjustments.
Symptoms of SLE
The symptoms of Systemic Lupus Erythematosus (SLE) can vary widely among individuals and may come and go. Here are common symptoms associated with SLE, presented in bullet points:
- Joint pain and swelling
- Fatigue and weakness
- Skin rashes, often in a “butterfly” pattern across the cheeks and nose
- Photosensitivity (increased sensitivity to sunlight)
- Fever
- Mouth sores
- Hair loss
- Raynaud’s phenomenon (fingers and toes turning white or blue in response to cold or stress)
- Chest pain and shortness of breath (if the heart or lungs are affected)
- Kidney problems (may manifest as changes in urine, swelling, or high blood pressure)
- Cognitive dysfunction or memory problems
- Blood disorders, such as anemia or low platelet count
- Positive antinuclear antibodies (ANA) test in blood tests
Definition of Lupus Nephritis
Lupus Nephritis is a specific manifestation of Systemic Lupus Erythematosus (SLE) that involves inflammation of the kidneys. In this condition, the immune system, which is overactive in individuals with SLE, mistakenly attacks the kidneys, leading to inflammation that can impair their function. Lupus Nephritis can range from mild to severe and, if left untreated, may cause long-term kidney damage.
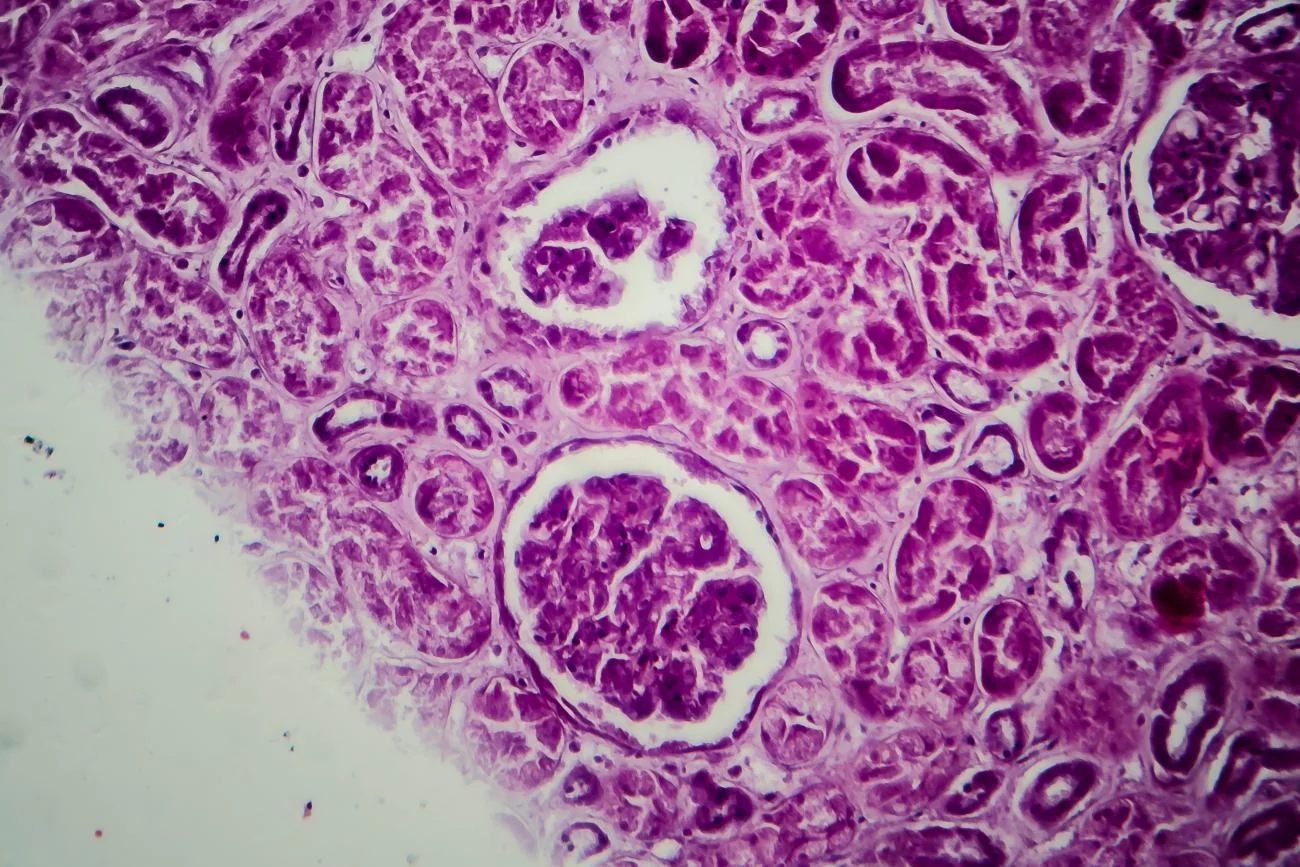
Common symptoms include swelling, high blood pressure, and changes in urine, such as blood or protein. Early detection and management of Lupus Nephritis are crucial to preserving kidney function and preventing complications.
Treatment often involves immunosuppressive medications to control the immune system’s activity and reduce inflammation in the kidneys. Regular monitoring and collaboration between rheumatologists and nephrologists are essential for effectively managing Lupus Nephritis in the context of systemic lupus.
Symptoms of Lupus Nephritis
Lupus Nephritis is a specific manifestation of Systemic Lupus Erythematosus (SLE) that involves inflammation of the kidneys. Here are some common symptoms associated with Lupus Nephritis, presented in bullet points:
- Swelling (edema), particularly in the legs, ankles, or around the eyes
- High blood pressure
- Changes in urine, including:
- Blood in the urine (hematuria)
- Foamy or frothy urine
- Increased or decreased urine production
- Dark urine
- Frequent urination, especially at night
- Proteinuria (excessive protein in the urine)
- Elevated levels of creatinine and urea in blood tests, indicating impaired kidney function
- Fatigue
- Joint pain
- Fever
- Headaches
- Rashes (may be related to the underlying SLE)
Comparison table of SLE and Lupus Nephritis
| Feature | Systemic Lupus Erythematosus (SLE) | Lupus Nephritis |
| Definition | Chronic autoimmune disease affecting multiple organs and tissues | Specific manifestation of SLE involving inflammation of the kidneys |
| Involvement | Can affect various systems (skin, joints, kidneys, etc.) | Primarily affects the kidneys |
| Symptoms | Diverse symptoms, including joint pain, skin rashes, fatigue, and inflammation | Symptoms may include swelling, high blood pressure, and changes in urine (blood or protein) |
| Cause | Combination of genetic, environmental, and hormonal factors | Result of the immune system mistakenly attacking the kidneys in individuals with SLE |
| Diagnosis | Based on a combination of clinical symptoms, blood tests (antibodies), and sometimes biopsy | Diagnosed through clinical evaluation, blood and urine tests, and often confirmed by kidney biopsy |
| Treatment | Management involves medications to control symptoms and prevent flare-ups, lifestyle adjustments | Treatment includes immunosuppressive medications to control immune system activity and reduce kidney inflammation |
| Prognosis | Varies widely; can be unpredictable and may require ongoing management | Prognosis depends on the severity, early detection, and effective treatment to prevent long-term kidney damage |
| Collaboration | Multidisciplinary approach involving rheumatologists, various specialists | Collaboration between rheumatologists and nephrologists for comprehensive management |
This table provides a concise comparison between Systemic Lupus Erythematosus (SLE) and Lupus Nephritis, highlighting key features such as definition, involvement, symptoms, cause, diagnosis, treatment, prognosis, and the need for collaboration in their management. Keep in mind that individual cases may vary, and consultation with healthcare professionals is essential for accurate diagnosis and personalized treatment.
What are the similarities between SLE and Lupus Nephritis?
Systemic Lupus Erythematosus (SLE) and Lupus Nephritis share several similarities, primarily because Lupus Nephritis is a specific manifestation of SLE. Here are some commonalities between the two:
- Autoimmune Origin: Both SLE and Lupus Nephritis are autoimmune conditions. In SLE, the immune system mistakenly attacks various tissues and organs throughout the body, while in Lupus Nephritis, the immune system targets and inflames the kidneys specifically.
- Inflammation: Both conditions involve inflammation. In SLE, inflammation can affect multiple systems, leading to diverse symptoms, and in Lupus Nephritis, the kidneys experience inflammation, potentially impairing their function.
- Overlap in Symptoms: While Lupus Nephritis has its specific symptoms related to kidney involvement (e.g., swelling, high blood pressure, changes in urine), there can be an overlap in symptoms with SLE, such as fatigue, joint pain, and skin manifestations.
- Chronic Nature: SLE and Lupus Nephritis are chronic conditions, meaning they are long-term and require ongoing management. Flare-ups and remissions are common in both, necessitating continuous monitoring and care.
- Diagnosis through Clinical Evaluation: The diagnosis of both SLE and Lupus Nephritis involves a combination of clinical evaluation, blood tests (including detection of specific antibodies), and, in the case of Lupus Nephritis, often a kidney biopsy.
- Treatment with Immunosuppressive Medications: The management of both SLE and Lupus Nephritis often includes the use of immunosuppressive medications to modulate the overactive immune response and reduce inflammation.
- Multidisciplinary Approach: Both conditions may require a multidisciplinary approach to management. In the case of SLE, various specialists (rheumatologists, dermatologists, etc.) may be involved, while Lupus Nephritis often involves collaboration between rheumatologists and nephrologists.
Understanding these similarities helps in recognizing the interconnected nature of SLE and Lupus Nephritis, emphasizing the need for a comprehensive and individualized approach to diagnosis and treatment.
Diagnosis of SLE and Lupus Nephritis
The diagnosis of Systemic Lupus Erythematosus (SLE) and Lupus Nephritis involves a combination of clinical evaluation, laboratory tests, and, in some cases, imaging or biopsies.
Here is an overview of the diagnostic process for both conditions:
Diagnosis of SLE
- Clinical Evaluation:
- A healthcare provider will assess the patient’s medical history, symptoms, and perform a physical examination.
- Blood Tests:
- Antinuclear Antibody (ANA) Test: Detects the presence of antibodies that target the cell nucleus, which is often elevated in SLE.
- Complete Blood Count (CBC): Checks for abnormalities in blood cell counts.
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): Indicators of inflammation.
- Autoantibody Tests: Including anti-dsDNA (anti-double-stranded DNA) and anti-Smith antibodies.
- Additional Tests:
- Urinalysis: To check for kidney involvement or abnormalities.
- Imaging: X-rays or other imaging studies may be done to assess joint or organ damage.
- Diagnostic Criteria:
- Diagnosis is often based on meeting certain criteria, such as those outlined by the American College of Rheumatology (ACR).
Diagnosis of Lupus Nephritis
- Clinical Evaluation:
- A rheumatologist or nephrologist will assess symptoms related to kidney function, such as swelling, changes in urine, and high blood pressure.
- Urine Tests:
- Urinalysis: Detects abnormalities such as proteinuria, hematuria, and other signs of kidney damage.
- Blood Tests:
- Blood tests to assess kidney function, including serum creatinine and blood urea nitrogen (BUN).
- Kidney Biopsy:
- In some cases, a kidney biopsy may be performed to confirm the diagnosis, assess the severity of kidney involvement, and guide treatment decisions.
- Imaging:
- Imaging studies, such as ultrasound or CT scans, may be used to visualize the kidneys and assess their structure.
Treatment for SLE and Lupus Nephritis
The treatment for Systemic Lupus Erythematosus (SLE) and Lupus Nephritis involves a combination of medications, lifestyle modifications, and, in the case of Lupus Nephritis, potential interventions to manage kidney involvement. Treatment plans are often individualized based on the severity of symptoms, organ involvement, and overall health. It’s crucial for patients to work closely with healthcare professionals, usually including rheumatologists and nephrologists, to manage these conditions effectively.

Treatment for SLE
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
- Used to manage mild joint pain and inflammation.
- Antimalarial Medications:
- Hydroxychloroquine is commonly prescribed to reduce symptoms and prevent flares.
- Corticosteroids:
- Prednisone or other corticosteroids may be used to reduce inflammation during flares.
- Immunosuppressive Medications:
- Medications such as azathioprine, mycophenolate mofetil, methotrexate, or cyclophosphamide may be prescribed to modulate the immune system and control disease activity.
- Biologic Therapies:
- Belimumab, a monoclonal antibody, may be used to specifically target B cells in certain cases.
- Sun Protection:
- Given the photosensitivity associated with SLE, patients are advised to use sunblock and protective clothing to minimize skin symptoms.
Treatment for Lupus Nephritis
- Immunosuppressive Medications:
- Corticosteroids are often used in combination with other immunosuppressive drugs like mycophenolate mofetil, azathioprine, or cyclophosphamide to control inflammation in the kidneys.
- Antihypertensive Medications:
- High blood pressure is common in Lupus Nephritis, and medications like ACE inhibitors or angiotensin II receptor blockers (ARBs) may be prescribed to manage blood pressure and protect the kidneys.
- Diuretics:
- Diuretics may be used to help manage fluid retention.
- Biologic Therapy:
- Some patients may be prescribed biologic medications, such as rituximab, which target specific components of the immune system.
- Lifestyle Modifications:
- Dietary changes, exercise, and smoking cessation may be recommended to improve overall health and manage risk factors.
- Regular Monitoring:
- Ongoing monitoring of kidney function, blood pressure, and overall health is crucial to assess the effectiveness of treatment and make adjustments as needed.
Treatment plans for both SLE and Lupus Nephritis are dynamic and may require adjustments over time. It’s essential for individuals with these conditions to communicate regularly with their healthcare team, adhere to prescribed medications, and adopt a healthy lifestyle to manage symptoms and minimize the impact on their quality of life.
Coping Strategies for Patients
Coping with Systemic Lupus Erythematosus (SLE) and Lupus Nephritis involves a combination of medical management, lifestyle adjustments, and psychological support.
Here are some coping strategies for patients dealing with these conditions:
Medical Management
- Adherence to Treatment:
- Strict adherence to prescribed medications and treatment plans is essential for managing symptoms and preventing flares.
- Regular Monitoring:
- Attend regular check-ups and laboratory tests as advised by healthcare professionals to monitor disease activity and treatment effectiveness.
Lifestyle Adjustments
- Balanced Diet:
- Adopt a well-balanced, nutritious diet to support overall health and possibly reduce inflammation. Consult with a healthcare professional or nutritionist for personalized dietary advice.
- Physical Activity:
- Engage in regular, low-impact exercises, such as walking or swimming, to maintain joint flexibility and overall well-being.
- Sun Protection:
- Minimize sun exposure by using sunblock, wearing protective clothing, and avoiding peak sunlight hours, especially for individuals with photosensitive skin.
- Stress Management:
- Practice stress-reducing techniques, such as mindfulness, meditation, or yoga, to help manage stress, which can trigger lupus flares.
Psychological Support
- Support Groups:
- Joining support groups for individuals with lupus can provide a sense of community, shared experiences, and emotional support.
- Therapy/Counseling:
- Consider seeking professional therapy or counseling to address the emotional and psychological impact of living with a chronic illness.
- Educate Yourself:
- Learn about your condition to empower yourself and better understand its management. Reliable sources include healthcare professionals, reputable websites, and patient education materials.
Lifestyle Modifications
- Adaptation:
- Adapt daily routines to conserve energy during periods of fatigue. Prioritize tasks and consider delegating responsibilities when needed.
- Sleep Hygiene:
- Establish a consistent sleep routine and create a comfortable sleep environment to support quality rest.
Social Support
- Communication:
- Communicate openly with family, friends, and colleagues about your condition, helping them understand the challenges you may face.
- Advocacy:
- Advocate for your needs within the healthcare system and workplace. Clear communication with healthcare providers and employers can help ensure appropriate accommodations and support.
Coping strategies can vary from person to person, and it’s crucial to tailor them to individual needs and preferences. Maintaining a positive mindset, seeking support when needed, and actively participating in your healthcare can contribute to better overall well-being for individuals with SLE and Lupus Nephritis.
Research and Innovations
Research and innovations in the field of lupus, including Systemic Lupus Erythematosus (SLE) and Lupus Nephritis, were focused on several areas:
- Precision Medicine:
- Researchers were exploring personalized treatment approaches based on an individual’s genetic makeup, immune system profile, and specific manifestations of the disease.
- Biologic Therapies:
- Continued development and testing of biologic drugs targeting specific components of the immune system, aiming to improve treatment efficacy with fewer side effects.
- Advanced Imaging Techniques:
- Innovations in imaging technologies, such as advanced MRI and ultrasound techniques, for more accurate and non-invasive assessment of disease activity and organ involvement.
- Biomarkers:
- Identification and validation of biomarkers that can serve as indicators for disease activity, severity, and potential treatment response.
- Stem Cell Therapy:
- Research into the use of stem cell transplantation as a potential treatment for severe cases of lupus, particularly Lupus Nephritis.
- Digital Health and Telemedicine:
- Integration of digital health tools and telemedicine to improve patient monitoring, adherence to treatment, and communication between patients and healthcare providers.
- Immunotherapy Approaches:
- Investigating immunotherapy strategies, including the use of regulatory T cells, to modulate the immune response and potentially induce long-term remission.
- Patient-Reported Outcomes:
- Emphasis on incorporating patient-reported outcomes and experiences in clinical trials to better understand the impact of treatments on quality of life and daily functioning.
- Genomic Studies:
- Large-scale genomic studies to identify genetic factors associated with lupus susceptibility, severity, and response to treatment.
- Microbiome Research:
- Exploring the role of the microbiome in lupus, with the aim of understanding how gut bacteria may influence the immune system and disease activity.
The field of medical research is dynamic, and new developments may have occurred since my last update. I recommend checking recent scientific literature, clinical trial databases, and reputable health organizations for the latest information on research and innovations related to lupus and Lupus Nephritis.
Conclusion
Systemic Lupus Erythematosus (SLE) is a chronic autoimmune disease that can affect various organs, including the kidneys. Lupus Nephritis is a severe manifestation of SLE, involving inflammation of the kidneys. Left untreated, it can lead to kidney damage and failure. Early detection and appropriate management are crucial in preventing irreversible harm. A multidisciplinary approach, combining medications and lifestyle modifications, is essential for managing both SLE and Lupus Nephritis to improve long-term outcomes and quality of life for affected individuals.