Gonococcal and nongonococcal urethritis, two forms of urethritis that involve inflammation of the urinary tract, differ by pathogen involved. Gonococcal urethritis is caused by Neisseria gonorrhoeae; while nongonococcal forms could involve bacteria, viruses or noninfectious factors.
Definition of urethritis
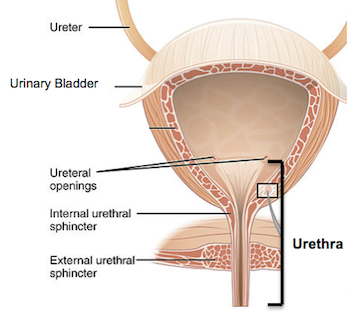
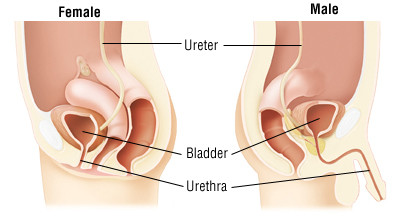
Urethritis, also referred to as Urethritis, refers to inflammation of the urethra (the tube that transports urine from your bladder out to your skin), which often results in both males and females and is caused by infections. Urethritis can be divided into several different subcategories depending on its source, including gonococcal (caused by Neisseria gonorrhoeae) and nongonococcal forms, both caused by various bacteria, viruses or noninfectious factors.
Condition characterized by symptoms including discomfort during urination and increased frequency, along with discharge from urethra. Early diagnosis and appropriate treatments can alleviate symptoms quickly while helping prevent complications and the spread of infections.
Different types of urethritis
There are primarily two main types of urethritis:
- Gonococcal Urethritis: Gonococcal urethritis is caused by infection with Neisseria gonorrhoeae bacteria, an sexually transmitted infection (STI). Transmission typically takes place through unprotected sexual contact between infected individuals. Gonococcal urethritis affects both males and females alike and often presents with painful urination, increased urinary frequency, yellow or greenish discharge from urethra, diagnosis verified through laboratory tests such as nucleic acid amplification tests (NAATs), Gram stain and culture results while antibiotic therapy should treat gonococcal urethritis effectively.
- Nongonococcal Urethritis (NGU): Nongonococcal Urethritis (NGU) refers to urethritis caused by microorganisms other than Neisseria gonorrhoeae; common examples being Chlamydia trachomatis and Mycoplasma genitalium as potential causes, while it could also arise due to chemical irritation or trauma. Similar symptoms exist as with gonococcal Urethritis including painful urination, increased urinary frequency, discharge from the Urethra as well as NAATs for diagnosis purposes while broad-spectrum treatment strategies should also be employed based on identification if identified; treatment should either directly targeting its specific causative agent(s), or at a minimum include broad-spectrum antibiotic treatment strategies with broad spectrum treatments as necessary (or both!).
Notably, other less frequent causes of urethritis include viral infections (e.g. herpes simplex virus) urinary tract infections and noninfectious conditions like urethral strictures – prompt diagnosis and appropriate treatment are therefore key components to successfully managing and avoiding complications related to urethritis.
Gonococcal Urethritis
Gonococcal urethritis is a type of urethritis caused by the bacterium Neisseria gonorrhoeae, commonly known as gonorrhea. It is a sexually transmitted infection (STI) that primarily affects the genital tract, including the urethra in males.
Key points about gonococcal urethritis:
Signs and Symptoms:
Signs and symptoms of gonococcal urethritis vary among individuals.
They most frequently include:
- Urethral Discharge: Gonococcal urethritis can be identified by its signature symptoms: yellow or greenish discharge from the urethra that may contain thick pus-like material.
- Painful Urination: Many individuals with gonococcal urethritis experience pain or a burning sensation when urinating. This discomfort is known as dysuria and is often one of the earliest symptoms.
- Frequent Urge to Urinate: Some people with gonococcal urethritis may feel the need to urinate more frequently than usual. However, the amount of urine passed may be relatively small.
- Redness and Swelling: The opening of the urethra (meatus) can become red, inflamed, and swollen due to the infection. This may cause discomfort or pain.
- Testicular Pain: Epididymitis can occur when infection spreads to a structure near the testicles called the epididymis and leads to swelling, tenderness and pain within them. In such an instance, painkillers will likely not suffice in relieving symptoms associated with epididymitis.
- Rectal Symptoms: If gonococcal urethritis is acquired through receptive anal intercourse, symptoms may include anal discharge, itching, discomfort, and pain during bowel movements.
- Sore Throat: In rare cases, if the infection is transmitted through oral sex, individuals may experience a sore throat and swollen tonsils.
Note that not everyone who becomes infected with Neisseria gonorrhoeae (the bacteria responsible for gonococcal urethritis) will develop symptoms. Asymptomatic infections are more common among women; even without obvious signs, infection may still spread sexually through sexual partners – so, if you suspect exposure or experience concerning symptoms it’s essential that medical evaluation and testing be sought immediately.
Diagnosis
Diagnostic criteria for gonococcal urethritis typically consist of reviewing medical histories, conducting physical exams and laboratory analysis to come to a diagnosis of gonococcal urethritis.
Here are the steps typically involved when diagnosing gonococcal urethritis:
- Medical History Assessment: Your healthcare provider will ask questions regarding your symptoms, sexual activity and possible exposures to sexually transmitted infections (STIs) such as gonorrhea. Accurate and detailed answers are crucial in order to provide an accurate diagnosis.
- Physical Examination: Healthcare provider will conduct a physical examination in order to detect visible signs of infection, such as checking genital area for discharge and any symptoms such as swelling or tenderness.
- Sample Collection: To confirm the diagnosis, laboratory tests are conducted. The healthcare provider will collect samples from the affected area for analysis. Depending on the specific situation, sample collection methods may include:
a. Urethral Swab: A swab is gently inserted into the urethra to collect a sample of discharge or cells from the infected site. This may cause some temporary discomfort but is usually tolerable.
b. Urine Sample: Under certain conditions, urine samples may be taken for analysis when there is no visible discharge but symptoms persist. This method may prove especially useful when there is no visible discharge but symptoms persist.
c. Rectal or Throat Swab: Whenever there is suspected gonococcal infection in either the rectum or throat area, swabs should be collected from these locations to test for presence of bacteria.
- Laboratory Testing: The collected samples are sent to a laboratory for analysis. The most common method for diagnosing gonococcal urethritis is through a test called nucleic acid amplification test (NAAT). NAATs detect the genetic material (DNA or RNA) of Neisseria gonorrhoeae bacteria. These tests are highly sensitive and specific.
- Dual Testing for Other STIs: Healthcare providers typically perform additional testing for other sexually transmitted infections (STIs), including chlamydia, since both infections often coexist together. Doing this helps ensure proper treatment is received and reduce the risk of complications.
It is important to remember that accurate diagnosis and treatment are crucial not only for your own health but also to prevent the spread of infection to others. If you suspect you have gonococcal urethritis or have been exposed to gonorrhea, it is recommended to seek medical attention promptly.
Treatment
Treatment for gonococcal urethritis usually entails taking antibiotics in order to eliminate the Neisseria gonorrhoeae bacteria responsible. To ensure complete eradication and reduced risks associated with antibiotic resistance, it’s vital that treatment continue as recommended, even if symptoms improve before completion of full course prescribed by healthcare professional.
Here are a few key points about gonococcal urethritis treatment:
- Antibiotic Therapy: The choice of antibiotics depends on several factors, including local resistance patterns and individual patient factors like allergies and previous treatment history. The most commonly recommended antibiotics for gonococcal urethritis include:
- Ceftriaxone: Due to increasing antibiotic resistance, injection antibiotics such as metronidazole have become the preferred therapy for gonorrhea treatment.
- Azithromycin or Doxycycline: These oral antibiotics may also be taken in addition to ceftriaxone in order to address possible co-infection with Chlamydia, as this occurs alongside Gonorrhea infections.
- Partner Treatment: It is crucial to inform and encourage all recent sexual partners to seek medical evaluation and treatment to prevent reinfection and further transmission. This practice, known as partner notification or contact tracing, helps interrupt the chain of transmission and protect both individuals and the broader community.
- Test of Cure: Once antibiotic treatment has been completed, it is advisable to undergo a follow-up test of cure to make sure it has effectively remedied an infection. The follow-up test involves retesting for Neisseria gonorrhoeae bacteria.
- Avoid Sexual Activity: To prevent reinfection and transmission during treatment, it is important to abstain from sexual activity or practice safe sex (e.g., using condoms) until both the infected individual and their sexual partners have completed treatment and received medical clearance.
- Alternative Treatments: In cases where the individual is allergic to the recommended antibiotics or if the infection is resistant to the first-line treatment, alternative antibiotics may be prescribed based on specific sensitivity testing.
Healthcare professionals should always be consulted in order to receive accurate diagnosis and effective treatment of gonococcal urethritis, taking individual circumstances and local guidelines into consideration in identifying an effective strategy for rapid resolution and reduction in symptoms as well as potential complications and further spread. Prompt and complete treatment not only helps alleviate symptoms quickly but can reduce complications caused by this infection as well as reduce further spread and spreading risks.
Prevention
Preventing gonococcal urethritis primarily involves adopting safe sexual practices and seeking regular testing for sexually transmitted infections (STIs).
Here are some important prevention measures:
- Practice Safe Sex: Consistent and correct use of condoms during sexual activity involving vaginal, anal and oral sex can significantly lower your risk of gonococcal urethritis. Condoms act as barriers against bacteria spread via bodily fluid exchange to keep gonococcal bacteria contained within our bodies in check.
- Limit Sexual Partners: Limiting the number of sexual partners and engaging in mutually monogamous relationships with those who have tested negative for sexually transmitted infections (STIs) can lower your risk of gonococcal urethritis. Keep in mind, however, that more sexual partners you have increases the chance of exposure to STIs.
- Get Regular STI Testing: It is essential to undergo regular testing for STIs, including gonorrhea, especially if you engage in high-risk sexual behavior or have multiple partners. Regular testing helps detect infections early and allows for prompt treatment, reducing the risk of complications and further transmission.
- Partner Communication: Open and honest communication with sexual partners about STIs, testing, and sexual health is crucial. Discussing past sexual history, testing status, and using protection can help make informed decisions and reduce the risk of transmission.
- Vaccination: At present, no vaccine specifically tailored towards gonococcal urethritis exists; however, vaccination against other sexually transmitted infections such as human papillomavirus (HPV) and hepatitis B can reduce your overall risk.
- Avoid Unprotected Sexual Contact: Engaging in unprotected sexual contact – such as vaginal, anal and oral sex – increases your risk for gonococcal urethritis. It should also be remembered that gonorrhea can spread not just via vaginal interaction but through both anal and oral encounters as well.
- Avoid Sharing Sex Toys: If you use sex toys, it is important to clean them thoroughly between uses or use barriers (such as condoms) to prevent the spread of bacteria and STIs.
- Screening and Treatment of Sexual Partners: If you are diagnosed with gonococcal urethritis, it is crucial to inform and encourage your recent sexual partners to seek medical evaluation and treatment. Treating sexual partners helps prevent reinfection and further transmission.
Remember, prevention is key when it comes to gonococcal urethritis and other STIs. Practicing safe sex, getting regular testing, and maintaining open communication with sexual partners are essential steps in protecting your sexual health and the health of others.
Public Health Implications
Gonococcal urethritis can have significant negative implications on public health due to its widespread prevalence, potential complications and antibiotic resistance strains that emerge as a result.
Here are the primary public health ramifications associated with gonococcal urethritis:
- High Prevalence and Transmission: Gonorrhea (including gonococcal urethritis ) is one of the most prevalent sexually transmitted infections worldwide and its high prevalence increases risk in communities and populations, especially where unprotected sexual activity takes place or when there are multiple partners present.
- Impact on Reproductive Health: Gonococcal urethritis can have devastating repercussions for both women and men alike. In women, an infection could spread into reproductive organs causing pelvic inflammatory disease (PID), with chronic pelvic pain, infertility and possible ectopic pregnancies being the results. On the male side, complications include epididymitis causing testicular damage leading to infertility or even damage that leads to testicular atrophy resulting in infertility or damage and infertility for them as a whole – something men rarely suffer from!
- Facilitates HIV Transmission: Gonococcal urethritis can increase the risk of acquiring or transmitting other sexually transmitted infections, including HIV. In the presence of gonorrhea, the risk of HIV transmission is amplified due to genital inflammation and an increased concentration of HIV target cells.
- Antibiotic Resistance: Neisseria gonorrhoeae, the bacteria responsible for gonococcal urethritis, has demonstrated an alarming ability to evolve resistance against antibiotics. Multidrug resistant strains of gonorrhea pose serious public health threats as their development limits treatment options and hinders efforts to control spread of infection – emphasizing the importance of appropriate antibiotic usage, antimicrobial stewardship practices and ongoing surveillance for resistance patterns.
- Screening and Contact Tracing: Public health agencies play a crucial role in implementing and promoting gonococcal urethritis screening programs. Routine screening of high-risk populations and individuals, as well as contact tracing to identify and notify sexual partners of infected individuals, are important strategies to interrupt the transmission chain and prevent further spread of the infection.
- Health Education and Promotion: Public health campaigns aimed at raising awareness about gonococcal urethritis, its symptoms, and the importance of safe sexual practices are essential. Educational initiatives can help increase knowledge about the infection, promote regular testing, encourage condom use, and emphasize the importance of seeking early medical care.
- Research and Development: Public health organizations and researchers continue investing in studies aimed at understanding the epidemiology, pathogenesis and antibiotic resistance mechanisms underlying gonococcal urethritis. Such work helps inform policy decisions, enhance diagnostic tools and facilitate development of new treatment strategies and vaccines.
Control and prevention efforts against gonococcal urethritis require joint efforts between healthcare providers, public health agencies, researchers, policymakers, community members and researchers. By employing effective prevention strategies such as responsible antibiotic use practices and raising awareness campaigns about their importance for public health initiatives can have an enormously positive effect in lessening its burden and associated complications.
Prompt diagnosis and appropriate therapy for gonococcal urethritis can help manage its complications while decreasing transmission rates of infection. Seeking medical assistance if symptoms indicate possible urethritis are present or exposure is confirmed is advised –
Nongonococcal Urethritis
Nongonococcal Urethritis (NGU) refers to any form of urethritis not caused by Neisseria gonorrhoeae bacteria; instead it typically results from other microorganisms, including Chlamydia trachomatis, Mycoplasma Genitalium Ureaplasma Urealyticum as well as other less prevalent bacteria or viruses; although chemical irritation or trauma to the urethra could also trigger it.
Key points about nongonococcal urethritis:
Causes and Risk Factors
A. Bacterial causes of NGU
- Chlamydia trachomatis: Chlamydia is the primary bacterial cause of NGU. As an sexually transmitted infection (STI), Chlamydia can invade and inflame your urethra, leading to symptoms including NGU.
- Mycoplasma genitalium: Mycoplasma genitalium is another bacterium that can cause NGU. It is also transmitted through sexual contact and can lead to urethral inflammation.
B. Viral causes of NGU
- Herpes simplex virus (HSV): While less common than bacterial causes, HSV can infect the urethra and cause symptoms resembling NGU.
- Human papillomavirus (HPV): Certain strains of HPV may lead to the development of genital warts and cause inflammation within the urinary tract.
C. Other potential causes and risk factors
- Sexual behavior: Engaging in unprotected sexual intercourse or having multiple sexual partners increases the risk of contracting NGU.
- Previous STI: A history of sexually transmitted infections, such as gonorrhea or syphilis, can increase the likelihood of developing NGU.
- Personal hygiene: Poor genital hygiene practices may contribute to the development of NGU.
- Sexual orientation: Men who have sex with men (MSM) have a higher risk of NGU due to specific sexual practices and a higher prevalence of certain STIs within this population.
- Age: NGU can affect individuals of any age, but it is more commonly seen in sexually active young adults.
D. Transmission modes of NGU
- Sexual transmission: NGU is primarily transmitted through sexual contact, including vaginal, anal, and oral sex.
- Vertical transmission: In some cases, NGU can be transmitted from an infected mother to her newborn during childbirth.
Note that NGU may have multiple causes and that pinpointing them all may prove challenging, making prompt diagnosis and treatment the key to avoiding complications or transmission to others.
Symptoms and Diagnosisc
A. Common symptoms of NGU
- Urethral discharge: White, yellow, or clear discharge from the urethra is a common symptom of NGU. The discharge may be thin or thick in consistency.
- Painful or burning sensation during urination: Many individuals with NGU experience discomfort or a burning sensation while urinating.
- Frequent urge to urinate: NGU can cause an increased frequency of urination.
- Urethral itching or irritation: Some people may experience itching or irritation in the urethral area.
- Inflammation and redness: The urethral opening may appear red and swollen in individuals with NGU.
B. Diagnostic methods and tests
- Medical history and physical examination: The healthcare provider will discuss the patient’s symptoms, sexual history, and perform a physical examination to assess for signs of NGU.
- Urine analysis: Urine samples may be collected and examined to detect white blood cells and bacteria present.
- Urethral swab: A swab may be inserted into the urethra to collect a sample of discharge for laboratory testing. This helps identify the specific cause of NGU, such as Chlamydia or Mycoplasma.
- Nucleic acid amplification tests (NAATs): NAATs are highly sensitive and specific tests used to detect the genetic material (DNA or RNA) of pathogens like Chlamydia and Mycoplasma.
- Testing for other STIs: Since NGU may be caused by various pathogens, additional tests for other sexually transmitted infections may also be recommended – these tests include those for gonorrhea, syphilis, herpes and HIV.
C. Differential diagnosis of NGU
- Gonorrhea: The symptoms of NGU can overlap with those of gonorrhea. Testing is necessary to differentiate between the two conditions.
- Urinary tract infection (UTI): UTIs can cause similar urinary symptoms as NGU, but they are caused by different bacteria and require specific treatment.
- Allergic reactions or irritants: Some individuals may experience urinary symptoms due to allergic reactions or irritants like soap, lotions and spermicides; therefore this should be factored into any diagnosis process.
Accurate diagnosis of NGU is essential to provide appropriate treatment and prevent complications. It is recommended to consult a healthcare professional for evaluation and testing if symptoms suggestive of NGU are present.
Complications and Long-Term Effects
A. Potential complications associated with NGU
- Epididymitis: In some cases, the infection from NGU can spread to the epididymis, a coiled tube located at the back of the testicle. This can lead to epididymitis, characterized by testicular pain, swelling, and discomfort.
- Reactive arthritis: Reactive arthritis is a possible complication of NGU, especially if the underlying cause is Chlamydia. It can cause joint pain, swelling, and inflammation, primarily affecting the joints of the lower extremities.
- Pelvic inflammatory disease (PID): Although not as prevalent, NGU may progress from the urinary tract into women’s reproductive organs and cause PID, an infectious disorder which may inflame and damage reproductive structures including the uterus, fallopian tubes, ovaries or both, leading to infertility or even an ectopic pregnancy.
- Increased risk of HIV transmission: Having NGU can increase the risk of acquiring or transmitting HIV during sexual activity if one partner is HIV-positive.
B. Long-term effects on reproductive health
- Infertility: If NGU is left untreated or if complications such as PID occur, it can potentially lead to infertility in both men and women. Damage to the reproductive organs can impair fertility and make conception difficult.
- Scarring and strictures: Chronic inflammation from NGU can cause scarring and narrowing (strictures) of the urethra, leading to urinary problems and discomfort during urination.
C. Impact on sexual partners
- Transmission to partners: If NGU is caused by an infectious agent, such as Chlamydia or Mycoplasma, it can be transmitted to sexual partners during unprotected sexual contact. Prompt diagnosis, treatment, and partner notification are essential to prevent further transmission.
- Shared risk factors: NGU can indicate the presence of other sexually transmitted infections. Sexual partners of individuals with NGU may also be at increased risk of other STIs and should undergo appropriate testing and treatment.
As soon as symptoms of NGU appear, seeking medical assistance immediately should be sought in order to protect reproductive health and avoid complications. Early diagnosis and treatment will help mitigate potential long-term consequences while decreasing transmission risks to others.
Treatment and Management
A. Antibiotic therapy for NGU
- Empiric treatment: In cases of NGU where the specific pathogen is unknown, empirical antibiotic therapy is usually initiated. This typically involves a regimen that covers the most common bacterial causes, such as Chlamydia and Mycoplasma. Azithromycin or doxycycline are commonly prescribed antibiotics for NGU treatment.
- Targeted treatment: If the causative organism is identified through diagnostic testing, specific antibiotic therapy may be prescribed. For example, if Mycoplasma genitalium is identified, treatment with antibiotics like azithromycin or moxifloxacin may be recommended.
B. Treatment considerations for specific causes
- Chlamydia trachomatis: Chlamydia is one of the primary causes of NGU. Treatment typically entails antibiotics like azithromycin or doxycycline; sexual partners should also undergo testing and be given appropriate therapy in order to prevent reinfection.
- Mycoplasma genitalium: If Mycoplasma genitalium is identified as the source of NGU symptoms, antibiotics such as azithromycin and moxifloxacin may be necessary for effective treatment. It’s essential that patients adhere to any recommended treatment plans and finish all courses of antibiotics completely.
C. Partner notification and treatment
- Contact tracing: Individuals diagnosed with NGU should inform their sexual partners about the infection so that they can be tested and treated if necessary. This helps prevent reinfection and further transmission of the infection.
- Testing and treatment for partners: Sexual partners of individuals with NGU should undergo testing for STIs, including Chlamydia, Mycoplasma, and other relevant pathogens. They should be treated if infections are detected.
D. Follow-up care and prevention of recurrence
- Follow-up testing: After completing antibiotic treatment, follow-up testing may be recommended to ensure the infection has been cleared.
- Safe sexual practices: Practicing safe sex, including consistent and correct condom use, can reduce the risk of acquiring or transmitting NGU and other STIs.
- Regular testing and screening: Regular STI testing is important, especially for individuals at higher risk, such as those with multiple sexual partners or engaging in high-risk sexual behaviors.
It is crucial to complete the prescribed course of antibiotics, even if symptoms improve, to ensure the infection is fully treated. Compliance with treatment and partner notification are essential for successful management of NGU and preventing its recurrence.
Prevention
A. Safe sexual practices
- Consistent condom use: Correct and consistent use of condoms during vaginal, anal, and oral sex can help reduce the risk of NGU and other sexually transmitted infections (STIs).
- Mutual monogamy: Engaging in sexual activity within a mutually monogamous relationship, where both partners have been tested and are known to be uninfected, can lower the risk of acquiring NGU and other STIs.
- Limiting sexual partners: Having fewer sexual partners can decrease the likelihood of exposure to potential infections and reduce the risk of NGU.
B. Use of barrier methods
- Dental dams: When engaging in oral sex, using dental dams can provide a barrier and reduce the risk of transmitting or acquiring NGU and other STIs.
- Gloves: When engaging in manual stimulation or any activity involving potential contact with bodily fluids, using gloves can offer protection against NGU and other STIs.
C. Regular testing and screening
- STI testing: Regular testing for STIs, including Chlamydia and other potential causes of NGU, is crucial, especially for individuals who are sexually active or have multiple sexual partners.
- Screening for asymptomatic infections: Since NGU can occur without noticeable symptoms, routine screening for STIs can help identify infections early and prevent complications.
D. Education and communication
- Knowledge sharing: Educate yourself and your sexual partners about NGU, other STIs, and safe sexual practices to make informed decisions.
- Open communication: Discuss sexual health with your partners, including past STI history, testing, and prevention strategies. Open communication can help ensure that both partners are aware of their risk factors and can take appropriate precautions.
By practicing safe sex, utilizing barrier methods, undergoing regular testing, and promoting open communication, individuals can significantly reduce the risk of acquiring NGU and other STIs. Prevention plays a crucial role in maintaining sexual health and well-being.
Outlook and Prognosis
A. Prognosis for NGU
- With appropriate and timely treatment, the prognosis for NGU is generally good. Most cases of NGU can be effectively treated with antibiotics.
- Prompt diagnosis and treatment help prevent complications and reduce the risk of long-term effects on reproductive health.
B. Importance of early diagnosis and treatment
- Early diagnosis and treatment of NGU are crucial to prevent the spread of infection to sexual partners and reduce the risk of complications.
- Appropriate treatment must be sought quickly to avoid persistent or recurrent symptoms and the risks of epididymitis or pelvic inflammatory disease (PID), along with lasting impacts to fertility. Delaying or inadequately treating fertility disorders could result in persistent symptoms as well as possible long-term consequences that threaten it.
C. Future research and advancements
- Ongoing research is focused on improving diagnostic techniques and identifying more accurate and rapid testing methods for NGU, including the detection of specific pathogens.
- Advances in understanding the microbial causes of NGU and their interactions with the human body may lead to the development of targeted therapies and more effective treatment options.
It is important to seek medical attention if symptoms suggestive of NGU are present. Following recommended treatment regimens, notifying sexual partners, practicing safe sex, and undergoing regular STI testing can help ensure a positive outlook and minimize the impact of NGU on one’s health and well-being.
It’s important to consult a healthcare provider for proper diagnosis and treatment if NGU is suspected. Prompt diagnosis and appropriate management of NGU are vital to alleviate symptoms, prevent complications, and reduce the risk of transmission to sexual partners.
Differences Between Gonococcal and Nongonococcal Urethritis
Distinguishing between gonococcal (GU) and nongonococcal urethritis (NGU) urethritis is essential in terms of diagnosis and treatment, with significant distinctions between each form.
Here are a few differences that set them apart:
- Causative Organisms:
- GU: Caused by the bacterium Neisseria gonorrhoeae, a sexually transmitted infection (STI).
- NGU: Caused by various microorganisms, including Chlamydia trachomatis, Mycoplasma genitalium, Ureaplasma urealyticum, and other less common bacteria or viruses.
- Epidemiology and Risk Factors:
- GU: More common in sexually active individuals and associated with high-risk sexual behaviors and multiple partners.
- NGU: Can occur in sexually active individuals of all genders, but certain pathogens like Chlamydia trachomatis are commonly associated with NGU.
- Clinical Features and Symptomatology:
- GU: Symptoms may include dysuria (painful urination), increased urinary frequency, and a yellowish or greenish discharge from the urethra.
- NGU: Symptoms are similar to GU and may include dysuria, increased urinary frequency, and a clear or cloudy discharge from the urethra. However, many cases of NGU are asymptomatic.
- Diagnostic Methods and Laboratory Tests:
- GU: Diagnosis is typically confirmed through laboratory tests, such as nucleic acid amplification tests (NAATs) or a Gram stain and culture, to detect and identify Neisseria gonorrhoeae.
- NGU: Diagnosis is made through NAATs to detect the presence of various causative organisms like Chlamydia trachomatis, Mycoplasma genitalium, or Ureaplasma urealyticum. Microscopic examination of urethral swabs may also be performed.
- Treatment Approaches:
- GU: Antibiotic therapy is the standard treatment for gonococcal urethritis. Commonly used antibiotics include ceftriaxone, often in combination with azithromycin or doxycycline.
- NGU: Treatment involves antibiotic therapy targeted at the identified or suspected causative organisms. Empiric treatment with broad-spectrum antibiotics like azithromycin or doxycycline may be initiated if a specific pathogen is not identified.
- Prognosis and Potential Complications:
- GU: If left untreated, gonococcal urethritis can lead to complications such as epididymitis, prostatitis, and urethral strictures.
- NGU: Nongonococcal urethritis may result in infection spreading to other parts of the reproductive system and leading to pelvic inflammatory disease in females as well as creating potential fertility issues.
Understanding the differences between gonococcal and nongonococcal urethritis helps healthcare providers determine the appropriate diagnostic tests and select the most effective treatment regimens. Prompt diagnosis, treatment, and partner notification are crucial to manage these conditions, prevent complications, and reduce the transmission of sexually transmitted infections.
Comparison chart
Here is a comparison chart highlighting the key differences between gonococcal urethritis (GU) and nongonococcal urethritis (NGU):
| Topics | Gonococcal Urethritis (GU) | Nongonococcal Urethritis (NGU) |
|---|---|---|
| Caused by | Neisseria gonorrhoeae (bacterium) | Various microorganisms, including Chlamydia trachomatis, Mycoplasma genitalium, Ureaplasma urealyticum, and others |
| Epidemiology | Associated with high-risk sexual behaviors and multiple partners | Can occur in sexually active individuals; some pathogens (e.g., Chlamydia trachomatis) commonly associated with NGU |
| Symptoms | Dysuria, increased urinary frequency, yellowish or greenish urethral discharge | Dysuria, increased urinary frequency, clear or cloudy urethral discharge |
| Diagnostic Methods | Nucleic acid amplification tests (NAATs), Gram stain and culture | NAATs, microscopic examination of urethral swabs |
| Treatment | Antibiotics targeting Neisseria gonorrhoeae (e.g., ceftriaxone), often in combination with other antibiotics | Antibiotics targeted at identified or suspected causative organisms, or empiric treatment with broad-spectrum antibiotics |
| Complications | Epididymitis, prostatitis, urethral strictures | Spread of infection, pelvic inflammatory disease (PID) in females, potential fertility issues |
| Prevention | Safe sexual practices, including condom use, limiting sexual partners, regular STI screenings | Safe sexual practices, condom use, limiting sexual partners, regular STI screenings |
Similarities Between Gonococcal and Nongonococcal Urethritis
Although gonococcal and nongonococcal urethritis (GU and NGU respectively) vary with regards to causative organisms and clinical features, they share certain similarities.
Here are a few similarities:
- Symptoms: Both GU and NGU can present with similar symptoms, including dysuria (painful urination), increased urinary frequency, and urethral discharge. The nature of the discharge may vary, with GU typically causing a yellowish or greenish discharge, while NGU may lead to a clear or cloudy discharge.
- Transmission: Both GU and NGU are primarily transmitted through sexual contact, including vaginal, anal, and oral sex. They are considered sexually transmitted infections (STIs).
- Diagnostic Methods: While the specific laboratory tests may differ, both GU and NGU require diagnostic testing to confirm the presence of the causative organisms. Nucleic acid amplification tests (NAATs) are commonly used for both types to detect the genetic material of the pathogens in urine or swab samples.
- Treatment: Antibiotic therapy is the standard treatment approach for both GU and NGU. The choice of antibiotics may differ based on the causative organisms, but the goal is to eliminate the infection and relieve symptoms. In some cases, empiric treatment with broad-spectrum antibiotics may be initiated while awaiting test results.
- Complications: If left untreated, both GU and NGU can lead to complications. GU can result in epididymitis, prostatitis, and urethral strictures in males, while NGU can contribute to pelvic inflammatory disease (PID) in females, potentially leading to infertility and other reproductive health issues.
- Prevention: Prevention strategies for GU and NGU are similar and primarily focus on practicing safe sexual behaviors. Consistent and correct use of condoms, reducing the number of sexual partners, and regular STI screenings are essential preventive measures for both conditions.
Understanding the similarities between GU and NGU highlights the importance of prompt diagnosis, appropriate treatment, and preventive measures. It emphasizes the need for comprehensive sexual health education and awareness to promote safer sexual practices and reduce the transmission of these infections.
Conclusion
Accurate diagnosis and appropriate management of gonococcal (GU) and nongonococcal (NGU) urethritis are crucial. GU is caused by Neisseria gonorrhoeae bacteria while NGU may involve different pathogens like Chlamydia trachomatis, Mycoplasma genitalium, Ureaplasma urealyticum etc. The symptoms may resemble one another: dysuria, increased urinary frequency, discharge from both sources but many cases of NGU may even go undetected.