Hypoxia is a disease that is caused by a lack of oxygen supply to tissues in the body, which can lead to potential health issues. It may be caused by a variety of reasons, such as a lower level of oxygen in air lung disease, or a lack of circulation. The symptoms of hypoxia are breathing problems as well as confusion and organ damage if it is not treated.
Hypercapnia however is a condition that is defined by an increase in carbon dioxide (CO2) in blood. It is typically triggered when the body’s capacity to remove CO2 is impaired usually because of respiratory issues such as hyperventilation or lung diseases. Hypercapnia may cause symptoms like anxiety, confusion shortness of breath, and, in the most severe instances respiratory failure. Both hypercapnia and hypoxia are serious medical conditions that require prompt intervention and evaluation.
What is Hypoxia?
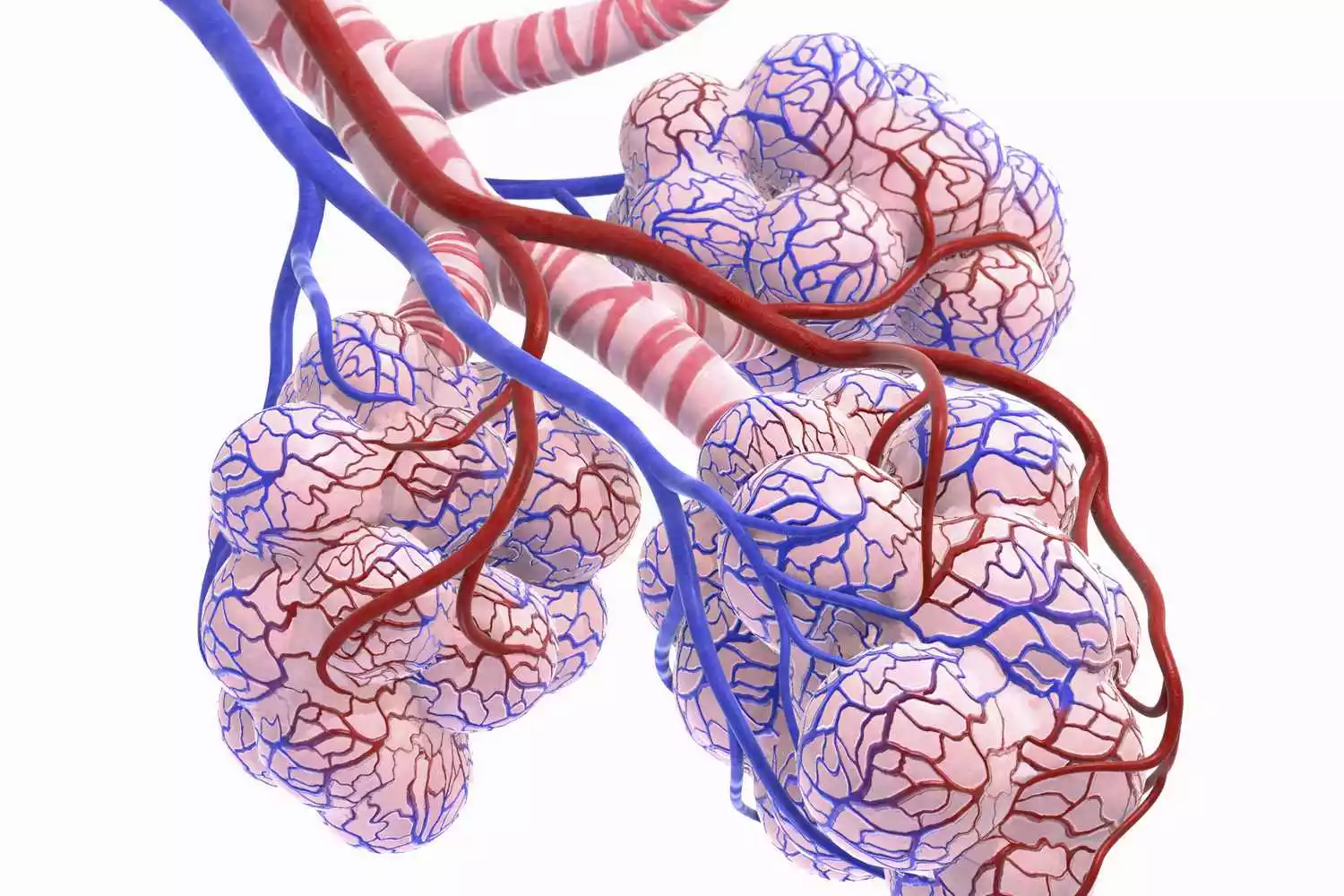
Hypoxia is a condition that is characterized by a lack of oxygen supply to organs and tissues of the body. It happens when there is an insufficient amount of oxygen present in the bloodstream that is sufficient to meet the body’s requirements for metabolism. Oxygen is vital to allow cells to perform their normal functions and create energy via a process known as cell respiration.
The cause of hypoxia is different factors, which include:
- Low Oxygen Levels in the Air: In environments with low oxygen levels, like high altitudes, or in enclosed spaces that have limited ventilation, some people can experience hypoxia.
- Respiratory problems: Conditions that impact your respiratory system including lung conditions (e.g. chronic obstructive lung disease, or COPD) as well as asthma or pneumonia, as well as a collapsed lung, may hinder the ability to breathe sufficient oxygen.
- Circulatory Issues: Issues in the circulatory or heart system could result in the inability of tissues to receive oxygen. The conditions like heart failure or severe anemia could cause hypoxia.
- Carbon Monoxide Poisoning: Inhalation of carbon monoxide (CO) which is an odorless and colorless gas that is produced through insufficient combustion of carbon-containing fuels could stop oxygen from binding to hemoglobin within the blood, which can cause hypoxia.
The symptoms of hypoxia could differ in severity and could include:
- Breathing shortness
- Rapid breathing
- Cyanosis (bluish or grayish skin especially on the nails and lips)
- Cognitive impairment or confusion
- Lightheadedness or dizziness
- Chest pain
- Headache
- Fatigue
- Weakness
What is Hypercapnia?
Hypercapnia is a medical issue that is characterized by the presence of elevated levels carbon dioxide (CO2) in blood. For healthy individuals the body is tightly regulating the level of CO2 via your respiratory system principally through exhaling excess CO2 every breath. However, many factors can cause a disruption to this balance, which can lead to the increase in carbon dioxide levels within the bloodstream.
Common causes of hypercapnia comprise:
- Respiratory Condition: These are conditions that affect the lungs, or the capacity to breathe properly may cause hypercapnia. For instance, chronic obstructive respiratory disease (COPD) as well as asthma as well as pneumonia and weakening of the respiratory muscle.
- Insufficiency in Ventilation: A decrease or impaired ventilation that could be caused by causes such as sedative medication and neuromuscular diseases, or an inability to breathe (as observed in certain neuromuscular disorders) and can result in being able to retain CO2.
- Occlusions of the Airway: Obstructions and obstructions to the airway, for instance the ones caused by tumors, or foreign objects, may stop CO2 exhalation and can cause hypercapnia.
The symptoms of hypercapnia may range from mild to serious and could include:
- Breathing shortness
- Rapid breathing
- Cognitive or confounding changes
- Headache
- Dizziness
- Flushed skin
- Muscle twitches or tremors
- Heart rate elevated
- A severe case can lead to respiratory failure which can be life-threatening situation.
Importance of knowing difference between Hypoxia and Hypercapnia
Understanding the difference between hypoxia and hypercapnia is crucial in medical practice, especially in critical care, respiratory therapy, and emergency medicine. Here’s why:
- Different Pathophysiology: Hypoxia and hypercapnia have different underlying mechanisms. Hypoxia is a lack of adequate oxygen supply to the tissues, while hypercapnia is an excess of carbon dioxide in the bloodstream. Each condition affects the body differently and requires a unique treatment approach.
- Symptom Recognition: Although both conditions can cause shortness of breath and fatigue, they present with different symptoms. Hypoxia often leads to cyanosis (bluish discoloration of the skin), confusion, and restlessness. Hypercapnia can cause flushed skin, drowsiness, headaches, and disorientation. Accurate symptom recognition is essential for appropriate diagnosis and treatment.
- Treatment Strategies: Treatment for hypoxia typically focuses on increasing oxygen delivery to the tissues, while the management of hypercapnia often revolves around improving ventilation to remove excess carbon dioxide. For instance, oxygen therapy is a primary treatment for hypoxia, but it must be used cautiously in patients with hypercapnia, especially in those with chronic obstructive pulmonary disease (COPD), to avoid suppressing their respiratory drive.
- Monitoring and Diagnosis: Monitoring methods such as pulse oximetry (which measures oxygen saturation) and arterial blood gas analysis (which measures both oxygen and carbon dioxide levels in the blood) are key in distinguishing between the two conditions.
- Risk of Complications: Each condition has its own set of potential complications. Chronic hypoxia can lead to organ damage, while chronic hypercapnia can result in respiratory acidosis, which can disturb the body’s acid-base balance and lead to further health issues.
- Underlying Causes: Identifying the cause of hypoxia or hypercapnia can lead to the diagnosis of different underlying conditions. For example, hypoxia may be due to pulmonary conditions like pneumonia or pulmonary embolism, while hypercapnia might be seen in chronic obstructive pulmonary disease or neuromuscular disorders.
- Emergency Response: In acute settings, distinguishing between hypoxia and hypercapnia is critical for rapid and effective intervention. For instance, in cases of overdose with certain drugs that depress the respiratory system, hypercapnia might be a more significant concern than hypoxia.
Comparison Table of Hypoxia and Hypercapnia
Here’s a comparison table of hypoxia and hypercapnia:
| Characteristic | Hypoxia | Hypercapnia |
| Definition | Insufficient oxygen supply to body tissues. | Elevated levels of carbon dioxide (CO2) in the blood. |
| Primary Cause | Low oxygen levels in the body or air. | Retention of carbon dioxide in the bloodstream. |
| Common Causes | – Lung diseases (e.g., pneumonia, COPD)
– High altitudes – Poor circulation (e.g., heart failure) |
– Respiratory conditions (e.g., COPD, asthma)
– Decreased ventilation (e.g., sedation) – Airway obstructions (e.g., tumors) |
| Symptoms | – Shortness of breath
– Cyanosis (bluish skin) – Confusion or cognitive changes – Dizziness – Headache – Fatigue – Weakness |
– Shortness of breath
– Confusion or cognitive changes – Headache – Flushed skin – Tremors or muscle twitches – Elevated heart rate |
| Potential Complications | Organ damage if left untreated. | Respiratory failure in severe cases. |
| Treatment | – Supplemental oxygen | – Address underlying cause (e.g., treat respiratory condition) |
| – Treating underlying cause | – Mechanical ventilation (e.g., ventilator) if severe | |
| – Assisting with breathing (e.g., ventilator) | – Administering supplemental oxygen | |
| – Addressing circulatory issues (if relevant) | – Treating carbon monoxide poisoning (if applicable) | |
| Prognosis | Prognosis depends on the underlying cause. Prompt treatment is essential to prevent complications. | Prognosis depends on the underlying cause. |
Similarities between Hypoxia and Hypercapnia
Hypercapnia and hypoxia both are distinct conditions that have distinct causes, they have some commonalities:
- Respiratory Stress: Both hypoxia as well as hypercapnia can trigger respiratory distress. People suffering from these conditions might be afflicted by symptoms like breathlessness rapid breathing, shortness of breath, and a labored breathing.
- Cognitive and Confusional Changes: The two conditions can cause mental changes. Hypercapnia and hypoxia may result in confusion, disorientation and difficulties in at concentrating.
- Cyanosis: In hypercapnia severe and hypoxia people can develop the condition known as cyanosis. It is characterized by blue or grayish skin, especially on nails, the lip and the extremities. This coloration can be caused by an insufficient oxygenation of blood.
- Headache: A symptom called headache that can be experienced in both hypercapnia and hypoxia. It can be a result of fluctuations in the flow of blood as well as oxygen supply into the brain.
- Heart and Cardiovascular: Effects of these conditions can impact your cardiovascular system. Hypercapnia and hypoxia can result in an increase in heart rate, as the body seeks to make up for the carbon dioxide or oxygen imbalance.
- Severity and Complications: In the event of complications and severity, not treated, hypercapnia and hypoxia can result in extreme organ damage and complications. In extreme instances they could pose a life-threatening threat.
- Treatment Principles: While treatments for hypercapnia and hypoxia vary because of their different root causes, the concept of providing respiratory support is the same. In both instances medical intervention seeks to fix the issue and increase oxygenation or ventilation.
How to diagnosis methods of Hypoxia and Hypercapnia?
The process of diagnosing hypercapnia and hypoxia involves assessing the symptoms of a patient’s clinical along with medical history, as well as performing various tests to identify the root cause of these ailments.

These are the typical diagnostic techniques for hypercapnia and hypoxia:
Diagnosis of Hypoxia:
- Diagnostic Assessment: Healthcare professionals will conduct an extensive physical exam and evaluate the patient’s vital signs including the rate of breathing, heart rate and levels of oxygen saturation with an oximeter pulse.
- Medical history: The collection of information regarding the medical history of the patient including any existing lung issues heart issues, lung conditions as well as exposure to extreme altitudes can give valuable information.
- The Arterial Blood Gas (ABG) Analysis: This is a important test for diagnosing hypoxia. ABG analysis is a method to measure the levels of oxygen (PaO2) and carbon dioxide (PaCO2) in the blood of the arterial, which helps to determine the severity and causes of hypoxia.
- Chest X-rays as well as CT Scan: Images can detect lung disorders or conditions such as pneumonia, atelectasis or pulmonary edema which may cause hypoxia.
- Pulmonary Function Tests (PFTs): These tests assess lung function, which includes lung capacity, volume, and airflow. This test could help in identifying the underlying cause of lung conditions, such as chronic obstructive lung disease (COPD) as well as asthma.
Diagnosis of Hypercapnia:
- Clinical assessment: As with hypoxia an examination of the body and assessment of vital indicators are essential in determining hypercapnia. Healthcare professionals will look for indications of respiratory distress, as well as changes in mental health.
- Arterial blood gas (ABG) Analyse: ABG analysis is an essential diagnostic tool for hypercapnia. It analyzes the levels of carbon dioxide (PaCO2) and oxygen (PaO2) in blood vessels to detect elevated CO2 levels.
- Chest X-rays as well as CT Scan: The imaging studies can be conducted to determine problems with the structure or in lung conditions that contribute to hypercapnia.
- PFTs (PFTs): PFTs can aid in assessing lung function and help diagnose respiratory diseases that can lead to hypercapnia, for example chronic obstructive lung disease (COPD).
- Capnography: Capnography can be described as a non-invasive way to monitor the level of carbon dioxide breath exhaled. It is able to provide real-time data about CO2 levels and assess the efficacy of treatment.
- Sleep studies: In cases of hypercapnia-related sleep, the polysomnographic test (a test of sleep) might be required to assess the patterns of breathing in the patient during sleep.
- Assessment of Neurology: In some cases hypercapnia could be caused by neurological disorders that impact breathing. An examination of the brain could be necessary to determine the causes of these problems.
The exact method for diagnosing will be determined by the symptoms of the patient, their medical history, as well as the clinical symptoms. When the root cause of hypercapnia or hypoxia is established and the correct treatment strategies are identified, they are taken to treat the root cause and increase oxygenation and ventilation.
Treatment Approaches for Hypoxia and Hypercapnia
The treatment strategies for hypercapnia and hypoxia vary because of their distinct root reasons. Here are the most common treatment options for each condition:
Treatment for Hypoxia:
- Supplemental Oxygen: The main therapy for hypoxia is providing an additional oxygen source to boost the levels of oxygen in bloodstream. Oxygen therapy is given by a variety of methods including nasal cannulas and face masks or non-rebreather masks based on the severity of hypoxia.
- Address Underlying Cause: It is essential to determine and address the root reason for hypoxia. For instance, if the hypoxia is caused by pneumonia, antibiotics could be prescribed. If the issue is related to heart disease, medication and lifestyle adjustments to improve heart function could be required.
- Ventilation Assistance: In severe cases of hypoxia, when the patient is not able to keep adequate oxygen levels in their breathing, mechanical ventilators with the use of a ventilator could be required.
- Pulmonary Rehabilitation For people suffering from chronic respiratory diseases such as COPD, the pulmonary rehabilitation program can improve the function of the lungs along with overall physical fitness as well as reducing the chance of recurring hypoxia-related episodes.
Treatment for Hypercapnia:
- Address Basis Cause: The primary approach for treating hypercapnia is to determine and treat the root condition that causes the retention of carbon dioxide. This could include:
- Controlling respiratory disorders such as COPD or asthma by anti-inflammatory drugs and bronchodilators.
- The treatment of pneumonia or other lung infections using appropriate antibiotics.
- Treating neurological disorders or issues with the central nervous system that affect breathing.
- Ventilation support: In severe cases of hypercapnia when the ability of a person to breathe is seriously impaired Mechanical ventilation via ventilators could be needed to help breathe and lowering CO2 levels.
- Oxygen Therapy Beware: While providing supplemental oxygen may help increase blood oxygen levels in some patients with hypercapnia, it must be handled with caution and the supervision of a doctor. Oxygen levels that are high can hinder the respiratory drive in certain instances, which could lead to worsening hypercapnia. The decision to take oxygen should be taken by a doctor depending on the specific medical condition.
- Lifestyle and behavioral changes: Patients suffering from chronic hypercapnia and who suffer from sleep issues, could be benefited from lifestyle changes like weight control smoking cessation and changes to sleeping postures.
The treatment plans for hypercapnia and hypoxia needs to be tailored to each patient’s particular condition and requirements. It is essential to speak with a physician to conduct a thorough assessment and individualized treatment suggestions. In both cases, prompt diagnosis and treatment are essential to avoid complications and improve the patient’s overall health.
Advancement of Hypoxia and Hypercapnia in Treatment
The advancement of hypoxia and hypercapnia in medical treatment primarily involves understanding and managing these conditions more effectively. Hypoxia refers to a deficiency in the amount of oxygen reaching the tissues, while hypercapnia is an excess of carbon dioxide in the bloodstream. Both conditions can be critical and require timely intervention.
In the treatment of hypoxia, advancements include:
- Enhanced Monitoring: Improved techniques for monitoring blood oxygen levels, including pulse oximetry and arterial blood gas tests, allow for more accurate and timely detection of hypoxia.
- Oxygen Therapy: Advancements in oxygen delivery systems, such as high-flow nasal cannula oxygen therapy, provide more efficient and comfortable ways to increase oxygen levels in patients.
- Hyperbaric Oxygen Therapy: This involves breathing pure oxygen in a pressurized room or chamber and is used for certain types of hypoxia.
- Ventilation Strategies: In critical care, advanced mechanical ventilation strategies and modes are used to optimize oxygenation while minimizing lung injury.
For hypercapnia, advancements include:
- Non-Invasive Ventilation (NIV): NIV, such as CPAP (Continuous Positive Airway Pressure) and BiPAP (Bilevel Positive Airway Pressure), helps in reducing CO2 levels, especially in conditions like COPD (Chronic Obstructive Pulmonary Disease).
- Mechanical Ventilation: In severe cases, mechanical ventilation is used to regulate both oxygen and carbon dioxide levels in the blood.
- Medication Management: The use of medications to treat underlying causes of hypercapnia, such as bronchodilators, steroids, and antibiotics for respiratory infections.
- CO2 Removal Technologies: Extracorporeal CO2 removal systems are an emerging technology for managing severe hypercapnia.
Both conditions also benefit from advancements in the underlying understanding of respiratory physiology, leading to more targeted treatments. The approach to managing these conditions is often multifaceted, involving a combination of respiratory support, medication, and treatment of underlying causes.
Conclusion
Hypercapnia and hypoxia are two distinct but closely related medical conditions that cause imbalances of carbon dioxide and oxygen within the body and the body, in turn. Hypoxia is caused by an insufficient oxygen intake and can be caused by a variety of causes, such as respiratory diseases and circulatory issues. Hypercapnia on the other side, is caused by high levels of carbon dioxide because of poor respiration or respiratory problems.
Both of them can result in grave health problems and treatment entails fixing the root of the problem by providing supplemental oxygen or ventilatory support as needed, and taking care of each patient’s individual requirements to restore normal breathing and avoid complications. The early diagnosis and prompt treatment is essential to ensure the health of those who are affected by these ailments.