Anaphylaxis is a severe and potentially life-threatening allergic reaction that occurs rapidly after exposure to an allergen. It triggers a systemic response, affecting multiple organ systems, leading to symptoms such as difficulty breathing, rapid drop in blood pressure, skin reactions like hives, swelling, and gastrointestinal issues.
Immediate medical intervention, typically with epinephrine and emergency care, is crucial to manage anaphylaxis and prevent its progression to a life-threatening situation. Prophylaxis, on the other hand, involves preventive measures to minimize the risk of anaphylactic reactions, including allergen avoidance, carrying emergency medications (such as epinephrine auto-injectors), and educating individuals with known allergies on early recognition and management strategies to prevent severe reactions.
Anaphylaxis
Anaphylaxis is a serious and life-threatening allergic response, typically following exposure to allergens. It involves immediate and systemic immune reactions affecting multiple organs and systems throughout the body. Anaphylaxis can result in the release of various chemicals from immune cells resulting in widespread inflammation and constriction of blood vessels, with sudden swelling.
Common triggers of anaphylaxis include peanuts, tree nuts, and shellfish as well as medications (antibiotics and nonsteroidal anti-inflammatory drugs), insect stings (bees or wasps), latex products, or certain environmental elements – the reaction usually occurring within minutes to hours following exposure to allergen. Its symptoms usually become evident within minutes to hours following contact.
The symptoms of anaphylaxis can be severe and rapidly progress. They may include:
- Respiratory symptoms: Difficulty breathing, wheezing, shortness of breath, coughing, and throat tightness.
- Skin symptoms: Hives, itching, flushing, and swelling, particularly of the face, lips, tongue, and throat.
- Gastrointestinal symptoms: Nausea, vomiting, abdominal pain, and diarrhea.
- Cardiovascular symptoms: Rapid or weak pulse, low blood pressure, lightheadedness, fainting, and in severe cases, cardiac arrest.

Causes of Anaphylaxis
Here are some common causes of anaphylaxis:
- Food Allergies: Food allergies may trigger anaphylactic reactions in susceptible individuals. Common food allergens include peanuts, tree nuts (such as almonds, walnuts and cashews), shellfish, fish eggs milk soy and wheat to name just a few.
- Insect Stings: Bee stings, wasp stings, hornet stings and fire ant bites can produce severe reactions in some individuals – sometimes anaphylaxis is even an imminent risk! Venom from these insects injecting their poison can trigger severe allergic reactions in those exposed.
- Medications: Various medications can induce anaphylaxis in certain individuals. Antibiotics, such as penicillin and cephalosporins, are commonly associated with allergic reactions. Other drugs, including nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin, and certain intravenous medications, can also be triggers.
- Latex: Latex is an all-natural rubber compound found in products like gloves, balloons and condoms. Some individuals develop allergic reactions to latex proteins found within these items which could result in anaphylaxis symptoms during medical procedures or when using products containing latex products containing latex components.
- Exercise-Induced: Rarely, physical activity or exercise may lead to anaphylaxis; typically this happens when combined with certain foods or exposure to specific environmental conditions.
- Idiopathic: At times, anaphylaxis’ cause remains unclear and difficult to pinpoint; this condition is known as “idiopathic anaphylaxis,” making identification of its trigger more challenging than expected.
Anaphylaxis is a medical emergency requiring immediate action to respond appropriately. When symptoms indicate possible anaphylaxis, treatment with adrenaline should begin immediately to halt any allergic reaction by constricting blood vessels and opening airways while providing necessary supportive measures such as administering antihistamines and corticosteroids as needed.
Following any acute incident of anaphylaxis individuals often consult an allergist in order to identify triggers and develop management plans in order to avoid future episodes.

Prophylaxis
Prophylaxis refers to measures taken to decrease the risk of an illness or condition and its progression, typically within individuals at increased risk or with specific vulnerabilities. Interventions designed for prevention aim at mitigating future medical events in these individuals who might otherwise develop it.
Prophylactic strategies vary based on each situation and condition being addressed, but here are a few examples:
- Vaccinations and Immunizations: Vaccines are an increasingly popular preventative method against infectious disease. By administering harmless versions of pathogens or their components into the body, vaccines stimulate immunity against them – helping either protect from future infection or mitigate symptoms if contracted.
- Preemptive Medication Administration: Prophylactic medications may be given to those at a risk for certain medical conditions. Antimalarial drugs, for instance, may be taken by travelers visiting areas prone to malaria in order to protect themselves against its spread; or other treatments might help avoid migraine headaches or reduce blood clot risk among individuals living with specific medical issues.
- Surgical Prophylaxis: Before undergoing surgery, patients may receive prophylactic antibiotics to prevent surgical site infections. These medications are typically administered shortly before the surgery and discontinued afterward to minimize the risk of complications.
- Allergy and Asthma Management: Prophylaxis is also employed in managing allergies and asthma. Patients with known allergies may be advised to avoid allergens and take preventive measures, such as using allergy-proof bedding or carrying epinephrine auto-injectors. In the case of asthma, prophylactic medications, such as inhaled corticosteroids or leukotriene modifiers, may be prescribed to control inflammation and prevent asthma attacks.
Causes of Prophylaxis
- Infectious Diseases: Prophylaxis can help protect against infectious disease outbreaks or outbreaks by offering protection from specific pathogens like measles, influenza, hepatitis or pneumococcal. Furthermore, antimicrobial prophylaxis may also be recommended before certain surgeries and medical procedures to avoid surgical site infections or complications during anesthesia procedures.
- Blood Clotting Disorders: Prophylaxis is often used to prevent blood clot formation in individuals with a high risk of developing blood clots. This can include the use of anticoagulant medications, such as heparin or warfarin, in patients with a history of deep vein thrombosis (DVT), pulmonary embolism (PE), or certain cardiovascular conditions.
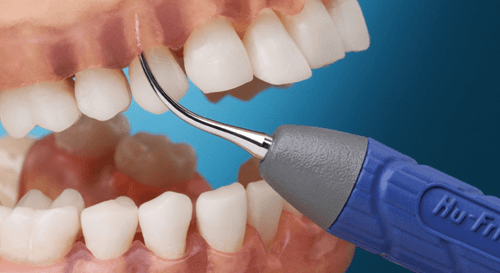
- Dental Care: Prophylactic measures in dental care involve preventative steps taken to maintain oral health and avoid dental diseases, including regular cleanings, fluoride treatments, sealants and education to guard against tooth decay, gum disease and other oral issues. This may include dental cleanings, fluoride applications and oral hygiene education as preventive tools against dental health concerns like decayed tooth enamel or diseased gums.
- Pre-Exposure Prophylaxis (PrEP): PrEP (Preventive Endogenous Retroviral Therapy) is an HIV infection preventative strategy used by those at increased risk, most notably individuals living in HIV-positive relationships or engaging in high-risk sexual practices, to lower their risks of disease infection and infection. Individuals at highest risk can take daily medication such as Tenofovir and Emtricitabine for this purpose.
- Occupational Exposures: Prophylactic interventions may be recommended for individuals at risk from occupational hazards. Healthcare workers, for example, could receive prophylactic vaccines and/or medications to guard against specific infections like Hepatitis B and Influenza.
- Genetic or Familial Risks: Prophylactic measures should be considered by individuals who have a genetic predisposition or family history of certain conditions, including regular screenings, lifestyle modifications or medications to lower risks or delay symptoms associated with breast cancer, colon cancer or cardiovascular diseases such as coronary artery disease.
Prophylactic measures offer numerous health advantages, including decreasing disease incidence and severity, mitigating complications, and improving overall health outcomes. When considering prophylaxis implementation options it is crucial to be mindful of any possible side effects or contraindications as well as conduct an individual risk-benefit analysis and seek medical advice regarding what interventions would best fit for specific scenarios.
Key Differences Between Anaphylaxis and Prophylaxis
Understanding the key differences between anaphylaxis and prophylaxis is important to differentiate the acute allergic reaction from preventative measures.
Here are the main distinctions between the two:
- Definition and Purpose:
- Anaphylaxis: Anaphylaxis refers to an acute allergic response which arises rapidly upon exposure to allergens. Anaphylaxis’ purpose is to address and manage an immediate allergic response as quickly as possible.
- Prophylaxis: Prophylaxis refers to preventative measures taken to lower your risk of disease or condition and has as its purpose the prevention or worsening of existing conditions or their progression before they manifest themselves.
- Timeframe and Onset:
- Anaphylaxis: Anaphylaxis occurs suddenly and has a rapid onset, usually within minutes to hours after exposure to the allergen.
- Prophylaxis: Prophylaxis refers to actions taken before any potential disease or condition has taken effect, to establish protective measures before they’re needed, including ongoing interventions or treatments regimens.
- Symptoms and Clinical Manifestations:
- Anaphylaxis: Anaphylaxis can manifest with acute symptoms that impact multiple organ systems and bodily systems simultaneously, including difficulty breathing, difficulty with swelling (hives or otherwise), low blood pressure, digestive distress or even cardiac arrest.
- Prophylaxis: Prophylaxis does not manifest with specific symptoms; rather it aims at preventing future episodes associated with certain illnesses or conditions.
- Diagnostic Criteria and Tests:
- Anaphylaxis: Anaphylaxis can be diagnosed by its clinical presentation and history of exposure. While skin prick tests and blood tests may help pinpoint specific allergens, they do not necessitate diagnosis in themselves.
- Prophylaxis: Prophylaxis does not entail specific diagnostic criteria or tests; rather, it requires an assessment of individual risk factors, medical history and guidelines in order to select preventative measures that suit you best.
- Treatment and Management Approaches:
- Anaphylaxis: Anaphylaxis requires immediate medical intervention and emergency measures, with treatment typically consisting of providing adrenaline (epinephrine) as the first-line response along with supportive care strategies and long-term management techniques.
- Prophylaxis: Prophylactic measures typically include vaccinations, medications or lifestyle modifications to avoid illness and condition in future cases. Specific strategies vary according to which disease or condition needs preventing, with approaches tailored specifically for each case being undertaken by prevention services.
- Target Population and Scenarios of Application:
- Anaphylaxis: Anaphylaxis can strike people who are sensitive or allergic to certain allergens in various settings – including food allergies, medication reactions or insect stings. It has the potential of becoming life threatening if left untreated and should always be managed carefully by medical practitioners.
- Prophylaxis: Prophylaxis can be applied to individuals who are at risk of developing a particular disease or condition. It can be utilized in various scenarios, such as immunizations for infectious diseases, medication administration before medical procedures, or lifestyle modifications to prevent chronic conditions.
Understanding these key differences helps distinguish anaphylaxis, an acute allergic reaction, from prophylaxis – preventative measures aimed at minimizing future episodes – as well as emphasize the significance of tailoring interventions based on specific context and goals of treatment.
Comparison chart
| Topics | Anaphylaxis | Prophylaxis |
|---|---|---|
| Definition | Severe and potentially life-threatening allergic reaction occurring rapidly after exposure to an allergen | Preventative measures taken to reduce the risk of developing a specific disease or condition |
| Purpose | Address and manage acute allergic response | Prevent the occurrence or progression of a condition before it happens |
| Onset | Sudden and rapid, typically within minutes to hours after exposure | Implemented before the potential disease or condition occurs |
| Symptoms | Severe and systemic symptoms affecting multiple organ systems | No specific symptoms – focuses on preventing symptoms associated with a particular disease or condition |
| Diagnosis | Based on clinical presentation and history of exposure to an allergen | No specific diagnostic criteria or tests |
| Treatment | Immediate medical attention and emergency measures, including administration of epinephrine | Interventions such as vaccinations, medications, or lifestyle modifications |
| Target Population | Individuals with known allergies or hypersensitivity to specific allergens | Individuals at risk of developing a particular disease or condition |
| Scenario | Acute allergic reactions triggered by allergen exposure | Preventing the onset or progression of diseases or conditions |
| Goal | Manage and mitigate acute allergic response | Minimize the risk of developing a specific disease or condition |
| Examples | Severe allergic reaction to peanuts or bee stings | Vaccinations, pre-surgical antibiotics, lifestyle modifications |
Similarities Between Anaphylaxis and Prophylaxis
While anaphylaxis and prophylaxis are distinct concepts with different purposes and applications, there are a few similarities between the two.
These include:
- Allergen Identification: An essential step in both anaphylaxis and prophylaxis treatment involves identifying any allergen or trigger that could be contributing to allergic reaction or condition being prevented; this process often includes reviewing medical histories, potential exposures and diagnostic testing as appropriate.
- Individualized Approach: Anaphylaxis and prophylaxis require personalized approaches for effective management, tailored specifically to each person based on medical history, triggers, risk factors and more. Healthcare providers assess each person as an individual to tailor the appropriate interventions accordingly.
- Risk Reduction: Both anaphylaxis and prophylaxis seek to minimize risks associated with allergic reactions or diseases or conditions by taking preventative steps, respectively. Anaphylaxis management seeks to minimize severe reactions during acute allergic attacks while prophylaxis seeks to limit development risk by adopting proactive preventive measures against particular ailments or ailments.
- Education and Preparedness: Both anaphylaxis and prophylaxis seek to minimize risks associated with allergic reactions or diseases or conditions by taking preventative steps, respectively. Anaphylaxis management seeks to minimize severe reactions during acute allergic attacks while prophylaxis seeks to limit development risk by adopting proactive preventive measures against particular ailments or ailments.
Noteworthy is the difference between anaphylaxis, emergency treatment for immediate allergic reactions, and prophylaxis focusing on prevention to decrease future incidence. While each approach differs significantly in terms of focus and outcome, their respective goals of improving health by mitigating risks and overall well-being remain similar.
Conclusion
Anaphylaxis and prophylaxis are two distinct concepts within healthcare. Anaphylaxis refers to an extreme and potentially life-threatening allergic reaction triggered by exposure to allergens; immediate medical attention and management of acute symptoms are required immediately for its management. Prophylaxis refers to preventative measures taken before an illness develops in order to lower its risk, with interventions implemented prior to any occurrence or progression occurring to reduce risks or potential risks of illness occurrence or progression.