Conn’s Syndrome and Pheochromocytoma are two distinct endocrine disorders associated with the adrenal glands. Conn’s Syndrome, or primary hyperaldosteronism, is characterized by excessive production of aldosterone, leading to high blood pressure, low potassium levels, and other metabolic disturbances. It is often caused by a benign adrenal tumor. Pheochromocytoma, in contrast, is a rare condition where a tumor, typically in the adrenal medulla, secretes high levels of catecholamines like adrenaline and noradrenaline. This results in episodes of high blood pressure, rapid heart rate, sweating, and anxiety. Both conditions are critical to diagnose and manage due to their significant impact on cardiovascular health.
Explanation of Conn’s Syndrome
Conn’s Syndrome, also known as primary hyperaldosteronism, is an endocrine disorder characterized by the excessive production of the hormone aldosterone by the adrenal glands. Aldosterone plays a crucial role in regulating sodium and potassium levels in the body.
In Conn’s Syndrome, this overproduction leads to an imbalance in these electrolytes, resulting in high blood pressure (hypertension), low potassium levels (hypokalemia), and sometimes alkalosis, a condition where the body fluids have an excessive alkaline (high pH) state.

Common symptoms include muscle weakness, fatigue, increased thirst and urination, and in some cases, heart palpitations. The condition is often caused by a benign tumor in one of the adrenal glands (adrenal adenoma) but can also result from other factors like bilateral adrenal hyperplasia. Left untreated, Conn’s Syndrome can lead to severe health complications, including cardiovascular disease.
Causes of Conn’s Syndrome
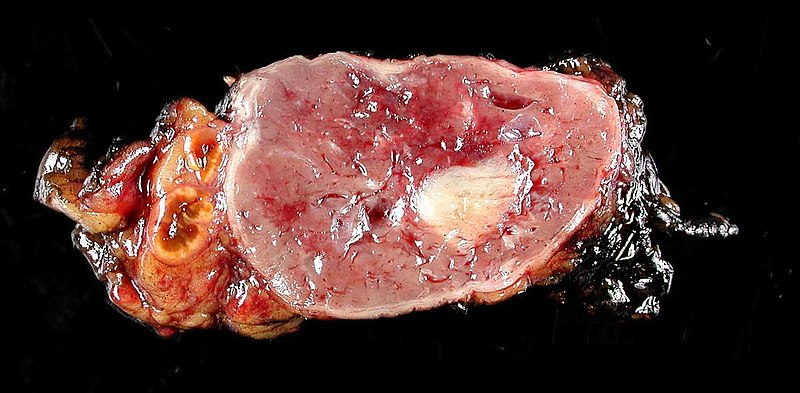
- Adrenal Adenoma: The most common cause of Conn’s Syndrome is the presence of a benign tumor in one of the adrenal glands, known as an adrenal adenoma. This tumor produces excess aldosterone.
- Bilateral Adrenal Hyperplasia: In some cases, both adrenal glands become enlarged and produce too much aldosterone.
- Familial Hyperaldosteronism: Rarely, genetic factors can lead to the condition, known as familial hyperaldosteronism.
- Other Causes: In very rare cases, Conn’s Syndrome may be caused by an adrenal carcinoma or other adrenal disorders.
Symptoms of Conn’s Syndrome
- High Blood Pressure: Often resistant to standard treatments.
- Muscle Weakness and Cramps: Due to low potassium levels.
- Fatigue: A common symptom due to electrolyte imbalances.
- Excessive Thirst and Urination: Resulting from the body’s attempt to balance sodium and potassium levels.
- Headache and Visual Disturbances: Related to high blood pressure.
- Numbness: Can occur sporadically.
Diagnosis of Conn’s Syndrome
- Blood Tests: To measure levels of aldosterone and renin. An abnormally high aldosterone-to-renin ratio suggests Conn’s Syndrome.
- Imaging Tests: CT scans or MRI of the adrenal glands to detect tumors or abnormalities.
- Salt Loading Test: To confirm the diagnosis; involves checking aldosterone levels after consuming a high-salt diet or receiving intravenous salt solution.
- Adrenal Vein Sampling: A specialized test to determine which adrenal gland is producing excess aldosterone.
Treatment Options for Conn’s Syndrome
- Surgery: If the condition is caused by a tumor, surgical removal of the affected adrenal gland may be recommended.
- Medications:
-
- Spironolactone or Eplerenone: These drugs block the action of aldosterone and are used if surgery is not an option or in bilateral adrenal hyperplasia.
- Calcium Channel Blockers and Other Antihypertensives: To manage high blood pressure.
- Lifestyle Changes: Including dietary modifications like reducing sodium intake and adopting healthy eating habits.
- Regular Monitoring: To keep track of blood pressure and electrolyte levels, especially potassium.
Management of Conn’s Syndrome is crucial to prevent complications such as heart disease, stroke, and kidney damage. The specific treatment approach depends on the underlying cause and the severity of the condition.
Explanation of Pheochromocytoma
Pheochromocytoma is a rare condition characterized by a tumor that usually develops in the adrenal medulla, the inner part of the adrenal glands. These tumors are known for producing excess amounts of catecholamines, specifically adrenaline and noradrenaline, which are hormones that regulate heart rate, blood pressure, and the body’s stress response.
The excessive release of these hormones typically leads to episodic or persistent high blood pressure, heart palpitations, headaches, sweating, and episodes of anxiety or panic. Other symptoms can include tremors, pallor, and a sense of doom. Although most pheochromocytomas are benign, they can cause significant health complications if not diagnosed and treated properly.
In some cases, the tumors can be malignant, potentially leading to more serious conditions. Pheochromocytoma can occur as a solitary condition or as part of a genetic syndrome, such as Multiple Endocrine Neoplasia type II or Von Hippel-Lindau disease.
Causes of Pheochromocytoma
- Adrenal Gland Tumors: Most pheochromocytomas originate from tumors in the adrenal medulla, the inner part of the adrenal gland.
- Genetic Factors: Certain inherited conditions, like Multiple Endocrine Neoplasia type II (MEN II), Von Hippel-Lindau disease, and Neurofibromatosis type 1, can increase the risk of developing pheochromocytoma.
- Sporadic Mutations: In many cases, pheochromocytomas occur sporadically, with no clear genetic or familial link.
- Extra-Adrenal Paragangliomas: Rarely, similar tumors called paragangliomas develop outside the adrenal glands but can cause similar symptoms.
Symptoms of Pheochromocytoma
- High Blood Pressure: Often severe and may be resistant to standard treatments.
- Heart Palpitations: Rapid, strong, or irregular heartbeats.
- Headache: Often severe and persistent.
- Sweating: Excessive sweating, particularly during episodes of high blood pressure.
- Anxiety or Panic Attacks: Feelings of extreme anxiety or panic.
- Tremors: Shaking or trembling episodes.
- Pallor: Pale skin, especially during episodes of symptoms.
- Abdominal Pain: Occurs in some cases.
Diagnosis of Pheochromocytoma
- Blood and Urine Tests: Measurement of catecholamines and metanephrines, which are elevated in pheochromocytoma.
- Imaging Tests: CT scans or MRI of the abdomen to visualize the adrenal glands and detect tumors.
- MIBG Scintigraphy: A specialized nuclear imaging scan that uses an iodine-labeled compound, which is taken up by adrenal tumors.
- Genetic Testing: Recommended for some patients, especially if there is a family history of related syndromes.
Treatment Options for Pheochromocytoma
- Surgical Removal: The primary treatment for pheochromocytoma is surgical removal of the tumor. Preoperative management to stabilize blood pressure and volume status is crucial.
- Medications:
-
- Alpha-Blockers: Used preoperatively to control blood pressure and prevent hypertensive crises.
- Beta-Blockers: May be added after alpha-blockers to control heart rate, but only once adequate alpha-blockade is achieved.
- Radiation Therapy or Chemotherapy: In cases of malignant or metastatic pheochromocytoma, these treatments may be considered.
- Lifestyle Modifications: Stress reduction and avoidance of known triggers that can provoke symptoms.
The management of pheochromocytoma is essential to prevent potentially life-threatening cardiovascular complications. Regular follow-up and monitoring are important, particularly in individuals with genetic predispositions or those with recurrent or malignant tumors.
Comparison table of Conn’s Syndrome and Pheochromocytoma
Here’s a comparison table highlighting the key differences between Conn’s Syndrome and Pheochromocytoma:
| Aspect | Conn’s Syndrome | Pheochromocytoma |
|---|---|---|
| Definition | A condition characterized by overproduction of aldosterone, leading to high blood pressure and low potassium levels. | A rare tumor in the adrenal medulla causing excess production of catecholamines, leading to high blood pressure and other symptoms. |
| Primary Cause | Often caused by an adrenal adenoma (benign tumor) or bilateral adrenal hyperplasia. | Usually caused by a tumor in the adrenal medulla, which may be benign or malignant. |
| Key Hormones Involved | Aldosterone. | Adrenaline and noradrenaline (catecholamines). |
| Common Symptoms | High blood pressure, muscle weakness, fatigue, increased thirst and urination. | High blood pressure, heart palpitations, headaches, sweating, anxiety or panic episodes. |
| Diagnosis | Blood tests for aldosterone and renin levels, imaging tests (CT or MRI), adrenal vein sampling. | Blood and urine tests for catecholamines, imaging tests (CT, MRI, MIBG scintigraphy). |
| Treatment | Surgery for adrenal adenoma, medications (spironolactone, eplerenone), lifestyle changes. | Surgical removal of the tumor, preoperative management with alpha-blockers, possibly radiation therapy or chemotherapy for malignant cases. |
| Potential Complications | Heart disease, stroke, kidney damage if untreated. | Cardiovascular complications, malignant transformation in rare cases. |
| Associated Conditions | May be part of familial hyperaldosteronism. | Can be associated with genetic syndromes like MEN II or Von Hippel-Lindau disease. |
This table provides a concise overview of the two conditions, highlighting their distinct features and management approaches.
Similarities between Conn’s Syndrome and Pheochromocytoma
Conn’s Syndrome and Pheochromocytoma, despite being distinct conditions, share several similarities:
- Adrenal Gland Involvement: Both conditions originate in the adrenal glands. Conn’s Syndrome is usually due to a problem in the adrenal cortex, while Pheochromocytoma originates from the adrenal medulla.
- Hormonal Imbalance: Each condition involves the overproduction of specific hormones. Conn’s Syndrome leads to excessive aldosterone production, whereas Pheochromocytoma is characterized by excess catecholamines (adrenaline and noradrenaline).
- High Blood Pressure: A common symptom for both disorders is hypertension. In Conn’s Syndrome, it’s due to aldosterone-induced sodium retention and potassium loss; in Pheochromocytoma, it’s caused by the overproduction of catecholamines.
- Diagnostic Process: Diagnosis of both conditions often involves blood tests (to measure hormone levels), urine tests, and imaging studies like CT scans or MRI to identify adrenal gland abnormalities.
- Treatment Involving Surgery: When a tumor is identified as the cause, surgical removal of the affected adrenal gland is a common treatment for both Conn’s Syndrome and Pheochromocytoma.
- Potential for Cardiovascular Complications: Untreated or poorly managed, both conditions can lead to serious cardiovascular complications due to persistent high blood pressure.
- Need for Long-term Monitoring: Both conditions require ongoing medical supervision post-diagnosis to manage symptoms, monitor hormone levels, and check for potential recurrence or complications.
These similarities highlight the importance of adrenal gland function in overall endocrine health and the interconnected nature of hormonal regulation in the body.
Future invention of Conn’s syndrome and pheochromocytoma in treatment
Predicting future advancements in the treatment of Conn’s Syndrome and Pheochromocytoma involves considering current trends in medical research and technology. While specific inventions or breakthroughs cannot be forecasted with certainty.
Here are some potential directions for future developments:
Conn’s Syndrome
- Gene Therapy: As our understanding of the genetic factors underlying Conn’s Syndrome improves, gene therapy could emerge as a potential treatment option, particularly for hereditary forms of the condition.
- Advanced Imaging Techniques: Improvements in imaging technology may lead to earlier and more precise detection of adrenal tumors or hyperplasia, allowing for more effective treatment planning.
- Targeted Drug Therapies: Development of medications that more specifically target the aldosterone-producing cells in the adrenal glands could provide a more effective treatment with fewer side effects.
- Non-Invasive Surgery Techniques: Advances in surgical techniques, such as robot-assisted surgery, may make the removal of adrenal tumors less invasive, reducing recovery times and improving outcomes.
Pheochromocytoma
- Personalized Medicine: As with many conditions, the future of treating Pheochromocytoma likely lies in personalized medicine, where treatments are tailored to the genetic and molecular profile of the individual’s tumor.
- Radiopharmaceutical Advances: Building on the current use of radiopharmaceuticals, future treatments may involve more effective and less toxic radioisotope therapies, potentially offering better control of metastatic or inoperable tumors.
- Immunotherapy: There is a potential for immunotherapy to play a role in treating Pheochromocytoma, especially if the tumor is malignant. This approach would harness the body’s immune system to target and destroy cancer cells.
- Advanced Molecular Targeting: Developing drugs that specifically target the molecular pathways involved in Pheochromocytoma growth and spread could provide more effective treatment options with fewer side effects.
General Trends
- Artificial Intelligence in Diagnosis: AI and machine learning could be used to analyze complex data from genetic, biochemical, and imaging sources to aid in early and accurate diagnosis.
- Wearable Health Monitoring: Advances in wearable technology may allow for continuous monitoring of vital signs in patients with these conditions, enabling better management of symptoms and treatment responses.
- Regenerative Medicine: Research in regenerative medicine, including stem cell therapy, might offer new ways to repair or regenerate adrenal tissue damaged by tumors or surgical removal.
The future of treating these adrenal gland disorders will likely be shaped by a combination of technological advances, deeper understanding of the diseases at a molecular level, and a more personalized approach to patient care.
Conclusion
Conn’s Syndrome and Pheochromocytoma are two distinct yet impactful conditions affecting the adrenal glands. Conn’s Syndrome, primarily characterized by the overproduction of aldosterone, leads to high blood pressure and electrolyte imbalances, posing risks of cardiovascular complications.
Pheochromocytoma, on the other hand, involves a tumor in the adrenal medulla causing excessive secretion of catecholamines, leading to episodic hypertension and a range of systemic symptoms. Both conditions demand precise diagnosis and careful management, often involving surgical intervention and long-term monitoring. Advancements in diagnostic techniques and treatment approaches continue to improve patient outcomes.
Understanding these conditions underscores the complexity of the endocrine system and the importance of targeted therapies in managing such specialized disorders.