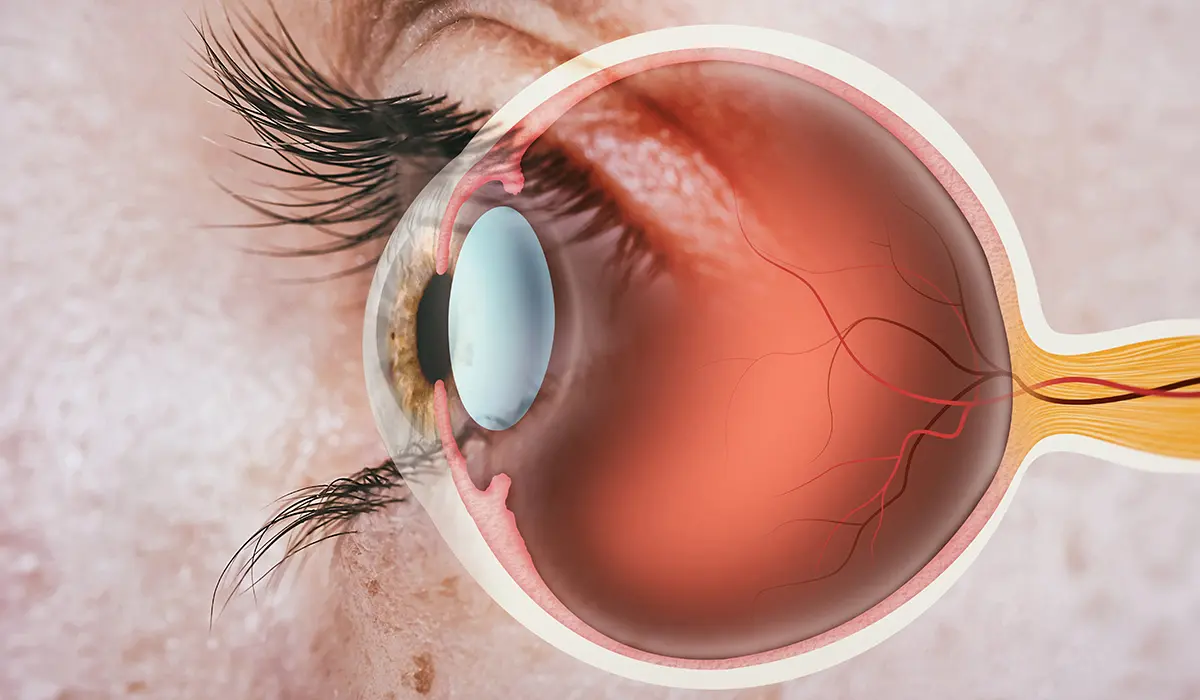
Glaucoma is a group of eye conditions that can cause blindness by damaging the optic nerve, typically due to abnormally high pressure in the eye, known as ocular hypertension. This pressure arises when the fluid that normally circulates in the front part of the eye cannot drain properly. Glaucoma often progresses slowly and without early symptoms, making regular eye exams crucial for early detection. Left untreated, it can lead to progressive vision loss and eventually blindness. Treatment often focuses on lowering eye pressure, using medications, laser treatment, or surgery, to slow or prevent further damage to the optic nerve.
What is Glaucoma?
Glaucoma is a group of eye diseases characterized by damage to the optic nerve, usually resulting from abnormally high pressure in the eye, known as intraocular pressure. This condition can lead to progressive vision loss and potentially blindness if not diagnosed and treated early. Glaucoma is often associated with a buildup of pressure inside the eye, which can occur when the eye’s fluid drainage system becomes less efficient with age or is blocked.
The increased pressure can then damage the optic nerve, which transmits images to the brain, leading to vision impairment. There are several types of glaucoma, with the most common being open-angle glaucoma, which typically progresses slowly and often without early symptoms. Early detection through regular eye exams is crucial, as glaucoma can be managed effectively with medications, laser treatment, or surgery if caught early.
Causes of Glaucoma
Glaucoma is caused by a range of factors, often related to increased pressure within the eye, which can damage the optic nerve. The specific causes and risk factors for glaucoma include:
- Increased Intraocular Pressure (IOP): The most common and significant risk factor for glaucoma is elevated pressure inside the eye. This pressure can damage the optic nerve, which is essential for vision.
- Aging: The risk of glaucoma increases with age, especially in individuals over 60.
- Ethnic Background: Certain ethnic groups, such as African-Americans, Hispanics, and Asians, have a higher risk of developing glaucoma.
- Family History: Genetics play a role in glaucoma, and having a family history of the condition increases one’s risk.
- Medical Conditions: People with certain medical conditions like diabetes, high blood pressure, and heart disease are at an increased risk of developing glaucoma.
- Eye Anatomy and Conditions: Those with naturally thin corneas, extreme nearsightedness or farsightedness, or past eye injuries are more susceptible to developing glaucoma. Conditions such as retinal detachment, eye tumors, and eye inflammations can also contribute to glaucoma.
- Use of Corticosteroids: Long-term use of corticosteroid medications, particularly in the form of eye drops, can increase the risk of secondary glaucoma.
- Blocked or Restricted Drainage in the Eye: In some forms of glaucoma, the eye’s drainage system becomes blocked or inefficient, leading to increased intraocular pressure.
- Reduced Blood Flow to the Optic Nerve: Poor blood flow or damage to the blood vessels feeding the optic nerve can contribute to glaucoma.
While elevated intraocular pressure is a significant risk factor, glaucoma can develop without increased eye pressure, known as normal-tension glaucoma. Regular eye examinations are essential for early detection and management of glaucoma, particularly for those at higher risk.
Symptoms of Glaucoma
Glaucoma often progresses stealthily and may not exhibit noticeable symptoms until significant vision loss has occurred. The symptoms can vary depending on the type and stage of glaucoma:
- Open-Angle Glaucoma (Chronic Glaucoma):
-
- Gradual Loss of Peripheral Vision: Typically in both eyes and often unnoticed until advanced.
- Tunnel Vision: In advanced stages, there might be a noticeable narrowing of the visual field.
- Angle-Closure Glaucoma (Acute Glaucoma):
-
- Severe Eye Pain: A rapid increase in eye pressure can cause intense pain.
- Nausea and Vomiting: Often accompanied by the severe eye pain.
- Blurred Vision: Sudden visual disturbance, often noticeable.
- Halos Around Lights: Seeing rainbow-colored circles around bright lights.
- Redness of the Eye: The eye may appear red due to the increased pressure.
- Headache: Can be quite severe.
- Sudden Visual Disturbance: Often in low light conditions.
- Normal-Tension Glaucoma:
-
- Slow Loss of Peripheral Vision: Similar to open-angle glaucoma but without elevated eye pressure.
- Developmental Glaucoma (Congenital Glaucoma):
-
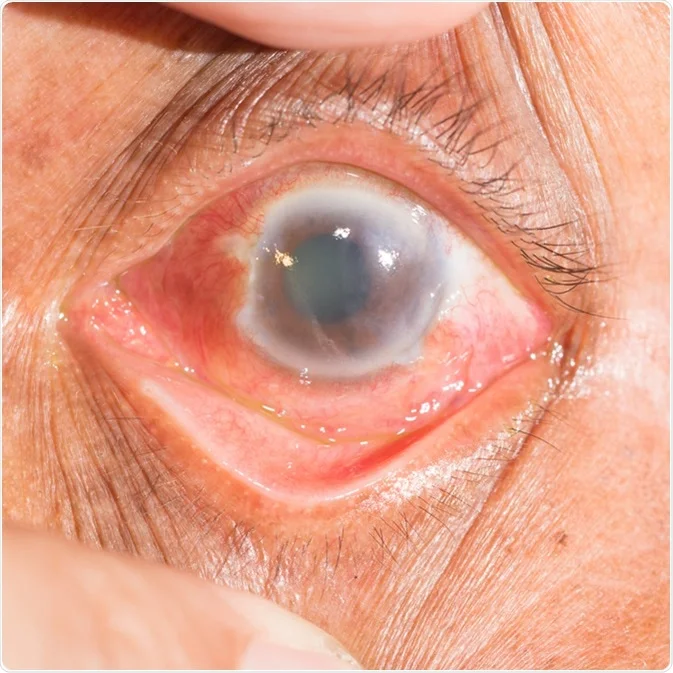
- Opacity of the Eye: The eye may appear cloudy.
- Enlargement of the Eye: More noticeable in infants.
- Sensitivity to Light: The child might be extremely sensitive to light.
- Excessive Tearing: An unusual amount of tearing.
Glaucoma is often called the “silent thief of sight” due to its subtle onset. Regular eye examinations are crucial for early detection, especially for individuals at higher risk, including older adults, those with a family history of glaucoma, and certain ethnic groups. Early detection and treatment can help preserve vision.
What is Ocular Hypertension?
Ocular hypertension refers to a condition where the pressure inside the eye, known as intraocular pressure (IOP), is higher than normal. Unlike glaucoma, which also involves high eye pressure but with associated optic nerve damage and vision loss, ocular hypertension does not by itself cause damage to the eyes or vision impairment. It is considered a significant risk factor for developing glaucoma.

Intraocular pressure is typically measured in millimeters of mercury (mmHg), and normal IOP ranges from 10 to 21 mmHg. Ocular hypertension is usually diagnosed when IOP consistently exceeds 21 mmHg without any detectable changes in vision or damage to the structures of the eye, including the optic nerve.
Regular eye exams are crucial for individuals with ocular hypertension, as they are at an increased risk of developing glaucoma. Monitoring the condition and managing the pressure through medications or other treatments can help reduce the risk of developing glaucoma and protect vision.
Causes of Ocular Hypertension
Ocular hypertension occurs when the pressure inside the eye, known as intraocular pressure (IOP), is higher than normal. The causes and risk factors for ocular hypertension include:
- Excessive Aqueous Production: The eye constantly produces a fluid called aqueous humor. If the eye produces an excessive amount of this fluid, it can lead to increased IOP.
- Inadequate Aqueous Drainage: Under normal conditions, aqueous humor flows out of the eye through a drainage system. If this drainage system becomes less efficient or is blocked, it can cause fluid to build up, leading to increased eye pressure.
- Eye Medications: Certain eye drops, particularly steroids, can increase intraocular pressure in some individuals.
- Eye Conditions and Diseases: Conditions such as eye trauma, uveitis (inflammation of the middle layer of the eye), and other eye disorders can lead to ocular hypertension.
- Genetic Factors: There is a hereditary aspect to ocular hypertension, meaning it can run in families.
- Age: The risk of ocular hypertension increases with age, particularly in people over 40.
- Ethnicity: Certain ethnic groups, such as African-Americans, are at a higher risk for ocular hypertension.
- Physical Attributes of the Eye: Individuals with naturally thinner corneas are at an increased risk for ocular hypertension.
Having ocular hypertension does not necessarily mean a person will develop glaucoma, but it is a significant risk factor. Regular eye exams are essential for monitoring and managing ocular hypertension to prevent potential complications, including the development of glaucoma.
Comparison table of Glaucoma and Ocular Hypertension
Here’s a comparison table outlining the key differences between Glaucoma and Ocular Hypertension:
| Aspect | Glaucoma | Ocular Hypertension |
| Definition | A group of eye diseases causing damage to the optic nerve, often associated with increased intraocular pressure. | Elevated intraocular pressure without associated damage to the optic nerve or vision loss. |
| Intraocular Pressure | Typically elevated, contributing to optic nerve damage. | Elevated, but without causing optic nerve damage or vision loss. |
| Optic Nerve Damage | Yes, damage to the optic nerve is a defining characteristic. | No, no evidence of optic nerve damage. |
| Vision Loss | Can lead to progressive vision loss and potential blindness. | No direct vision loss, but increased risk for developing glaucoma. |
| Symptoms | Often asymptomatic in early stages; can lead to peripheral vision loss, difficulty with night vision, and potential blindness in advanced stages. | Generally asymptomatic; detected through routine eye exams. |
| Risk Factors | Age, family history, high intraocular pressure, certain medical conditions like diabetes, and extreme nearsightedness. | High intraocular pressure, age, family history of glaucoma, certain ethnic backgrounds, and certain eye conditions. |
| Diagnosis | Comprehensive eye exam including measuring intraocular pressure, inspecting the optic nerve, and field of vision tests. | Diagnosed when intraocular pressure is consistently higher than normal (over 21 mmHg) in the absence of optic nerve damage or vision loss. |
| Treatment | Aimed at reducing intraocular pressure to prevent further optic nerve damage, using medications, laser therapy, or surgery. | Monitoring and regular eye exams; treatment may be considered to lower the risk of developing glaucoma. |
This table provides an overview of the differences and similarities between the two conditions. Regular eye exams are crucial in both cases for early detection and management.
Diagnosis Procedures of Glaucoma and Ocular Hypertension
The diagnosis of both glaucoma and ocular hypertension involves similar procedures, primarily focused on evaluating the health of the eye, particularly the optic nerve, and measuring intraocular pressure (IOP).

Key diagnostic procedures include:
- Tonometry: This test measures the intraocular pressure (IOP) of the eye. Elevated IOP is a significant indicator of glaucoma and is the defining feature of ocular hypertension.
- Ophthalmoscopy (Fundus Examination): This involves examining the optic nerve for glaucoma-related damage. The doctor uses eye drops to dilate the pupil and then examines the shape and color of the optic nerve.
- Gonioscopy: This test examines the angle in the eye where the iris meets the cornea. It’s particularly important for determining whether the angles are open or closed, which helps in distinguishing between open-angle and angle-closure glaucoma.
- Visual Field Test (Perimetry): This test maps the visual field, including peripheral vision, to check for any areas of vision loss. Glaucoma typically causes a loss of peripheral vision.
- Pachymetry: This simple, painless test measures the thickness of the cornea. Corneal thickness can influence eye pressure readings, and thin corneas can increase the risk of glaucoma.
- Optical Coherence Tomography (OCT): This non-invasive imaging test provides high-resolution images of the optic nerve and retina. It helps in assessing the thickness of the nerve fiber layer and identifying areas of thinning that might suggest glaucoma.
- Nerve Fiber Layer Analysis: Similar to OCT, this test evaluates the thickness of the nerve fiber layer around the optic nerve for signs of glaucoma.
In both glaucoma and ocular hypertension, regular monitoring is key. For glaucoma, it’s crucial to assess the progression of the disease and the effectiveness of treatment, while in ocular hypertension, it’s important to detect the potential onset of glaucoma. Early detection and ongoing management are essential for preserving vision and preventing further damage.
Treatment Approaches for Glaucoma and Ocular Hypertension
The treatment approaches for glaucoma and ocular hypertension primarily focus on lowering intraocular pressure (IOP) to prevent damage to the optic nerve and preserve vision.

The specific treatment strategies can vary based on the type and severity of the condition:
Treatment for Glaucoma:
- Medications: Prescription eye drops are often the first line of treatment. These can include prostaglandin analogs, beta-blockers, alpha agonists, carbonic anhydrase inhibitors, and rho kinase inhibitors. They work by either decreasing the production of fluid in the eye or increasing its outflow, thereby reducing IOP.
- Laser Therapy:
-
- Trabeculoplasty: Used for open-angle glaucoma, this procedure improves drainage outflow.
- Iridotomy: For angle-closure glaucoma, this creates a small hole in the iris to allow fluid to flow more freely.
- Surgery:
-
- Trabeculectomy: This involves creating a new drainage path to allow fluid to bypass the blocked drainage channels.
- Tube Shunt Surgery: Implants a tiny tube to help drain fluid and lower eye pressure.
- Minimally Invasive Glaucoma Surgery (MIGS): Offers a lower-risk alternative to traditional surgery, often with quicker recovery times.
Treatment for Ocular Hypertension:
- Observation and Monitoring: Not all cases of ocular hypertension require immediate treatment. Instead, regular monitoring of IOP and the optic nerve health may be recommended, especially if the risk of developing glaucoma is low.
- Medications: If the risk of developing glaucoma is significant, or if IOP reaches levels that could potentially damage the optic nerve, similar medications used for glaucoma may be prescribed.
- Lifestyle Changes: Advising on lifestyle modifications, such as regular exercise and a healthy diet, can sometimes help in managing IOP.
Common Elements in Treatment:
- Regular Follow-Up: Both conditions require ongoing monitoring to assess the effectiveness of the treatment and make adjustments as necessary.
- Individualized Treatment: The treatment plan is tailored based on individual risk factors, the severity of the disease, and patient response to treatment.
- Goal of Treatment: The primary goal is to maintain IOP at a level that reduces the risk of optic nerve damage, thereby preserving vision.
Early detection and consistent treatment are key in managing both glaucoma and ocular hypertension to prevent vision loss and maintain quality of life. Regular eye exams play a crucial role in the early identification and management of these conditions.
Lifestyle and Home Remedies
For individuals with glaucoma, ocular hypertension, or those at risk for these conditions, certain lifestyle and home remedies can complement medical treatments and help manage eye health. While these measures do not replace medical treatment, they can support overall eye health and potentially slow disease progression:
- Regular Exercise: Moderate, regular exercise can help reduce intraocular pressure in some cases. It’s important to avoid high-intensity exercises or activities that increase blood pressure, as they might increase intraocular pressure.
- Healthy Diet: A balanced diet rich in nutrients like vitamins C and E, omega-3 fatty acids, and antioxidants can contribute to overall eye health. Green leafy vegetables, fish, and fruits should be included in the diet.
- Limit Caffeine: Excessive caffeine consumption can potentially increase eye pressure, so it’s recommended to limit caffeine intake.
- Stay Hydrated: Drinking fluids in moderation throughout the day can prevent sudden increases in eye pressure that can occur with rapid fluid intake.
- Elevate the Head While Sleeping: Elevating the head by about 20 degrees while sleeping can reduce intraocular pressure during the night.
- Avoid Smoking and Limit Alcohol: Smoking and excessive alcohol use can adversely affect eye health. Quitting smoking and limiting alcohol consumption are beneficial for overall health and potentially for eye health as well.
- Wear Eye Protection: Protecting the eyes from injury, especially during sports or activities involving potential eye hazards, is important, as trauma can lead to increased eye pressure.
- Manage Stress: Chronic stress may impact intraocular pressure, so practicing stress management techniques like meditation, yoga, or deep breathing can be helpful.
- Compliance with Medication: For those prescribed medication for eye pressure, strict adherence to the prescribed regimen is crucial.
- Regular Eye Exams: Regular check-ups with an eye care professional are essential for monitoring eye health, especially for individuals at risk for or living with glaucoma or ocular hypertension.
These lifestyle adjustments and home remedies can be helpful in managing eye health, but they are most effective when used in conjunction with professional medical care. Always consult with a healthcare provider for personalized advice and before making significant changes to health routines.
Long-term Management and Monitoring
Long-term management and monitoring are crucial for conditions like glaucoma and ocular hypertension, as they can significantly impact vision and quality of life. Here are key strategies for effective long-term management:
- Regular Eye Examinations: Regular visits to an eye care professional are essential. The frequency of these visits depends on the severity and stability of the condition. For glaucoma patients, this might range from every 3-6 months, while for those with ocular hypertension, yearly exams may suffice.
- Consistent Use of Medications: If prescribed, it’s crucial to use eye drops or other medications exactly as directed. Inconsistencies in medication adherence can lead to fluctuations in intraocular pressure and may increase the risk of vision loss.
- Monitoring Intraocular Pressure (IOP): Regular IOP checks help in assessing the effectiveness of treatment and making necessary adjustments.
- Visual Field Testing: Regular visual field tests can help detect any changes or progression in vision loss due to glaucoma.
- Optic Nerve Assessments: Regular examinations of the optic nerve, often through imaging tests like Optical Coherence Tomography (OCT), can help monitor the health of the optic nerve and detect changes over time.
- Lifestyle Modifications: Maintaining a healthy lifestyle, including regular exercise, a balanced diet, managing stress, and avoiding smoking, can be beneficial in managing these conditions.
- Education and Support: Understanding the condition, its risks, and how to manage it is vital. Support groups or counseling can be beneficial for coping with the emotional aspects of chronic eye conditions.
- Home Monitoring: Some patients may benefit from home monitoring devices to check their IOP or visual field, though this should complement, not replace, professional examinations.
- Managing Comorbid Conditions: Conditions like diabetes and hypertension can impact eye health, so it’s important to manage these effectively.
- Regular Communication with Healthcare Providers: Keeping an open line of communication with healthcare providers is important for reporting any changes in vision or side effects from medications.
- Surgical Interventions (if necessary): In some cases, surgical procedures may be required. Regular follow-ups post-surgery are crucial to monitor for complications or recurrence of high IOP.
- Awareness of Symptoms: Knowing the symptoms that indicate worsening of the condition, like sudden vision changes or eye pain, and seeking immediate medical attention if they occur.
Long-term management of glaucoma and ocular hypertension is a collaborative process that involves the patient, eye care professionals, and often a primary care doctor. Regular monitoring and adherence to treatment plans are vital for preserving vision and managing these conditions effectively.
Impact on Quality of Life
The impact of glaucoma and ocular hypertension on quality of life can be significant, affecting various aspects of daily living:
- Visual Impairment: Progressive vision loss, particularly peripheral vision, can affect daily activities like reading, driving, and recognizing faces. Advanced glaucoma may lead to significant or total vision loss, profoundly impacting independence and lifestyle.
- Emotional and Psychological Impact: The diagnosis and progression of a chronic eye condition can lead to anxiety, depression, and a feeling of loss of control. The fear of eventual blindness can be particularly distressing.
- Mobility and Safety: Loss of peripheral vision and visual acuity can increase the risk of falls and accidents, making navigation in unfamiliar environments challenging and potentially dangerous.
- Social Interaction: Difficulty in visual perception can affect social interactions and communication. For example, recognizing facial expressions and non-verbal cues may become difficult, which can lead to social withdrawal.
- Occupational Challenges: Vision impairment can affect job performance, especially in professions requiring precise visual skills. This might lead to a need for job modification or even a change in career.
- Treatment Regimen: Adhering to a treatment regimen, especially with eye drops, can be cumbersome and easily forgotten. The side effects of medications, such as dry eyes or redness, can also be bothersome.
- Financial Burden: The cost of ongoing medical treatment, medications, and potentially surgery can be a significant financial stressor, especially for those without adequate health insurance coverage.
- Sleep and Daily Routines: Some glaucoma patients may need to adjust sleeping positions or modify daily routines to manage their condition, which can affect overall comfort and lifestyle.
- Coping with Uncertainty: Living with the uncertainty of disease progression and potential vision loss can be emotionally taxing.
- Dependency: As vision diminishes, reliance on others for daily tasks and transportation can affect one’s sense of independence and self-esteem.
While the impact on quality of life can be substantial, early detection and treatment, along with support from healthcare providers, family, and support groups, can help manage these challenges effectively. Adaptation strategies, use of visual aids, and lifestyle modifications can also significantly improve quality of life for individuals living with glaucoma or ocular hypertension.
Technological Advancements in Treatment
Technological advancements in the treatment of glaucoma and ocular hypertension have significantly improved patient outcomes and management strategies.

These advancements include:
- Minimally Invasive Glaucoma Surgery (MIGS): MIGS procedures offer a less invasive alternative to traditional glaucoma surgery, with fewer complications and a quicker recovery time. These techniques focus on reducing intraocular pressure by improving aqueous humor outflow.
- Advanced Imaging Techniques: Technologies like Optical Coherence Tomography (OCT) provide high-resolution images of the optic nerve and retinal fiber layers, aiding in early detection and precise monitoring of disease progression.
- Laser Therapy Enhancements: Newer laser therapies, such as Selective Laser Trabeculoplasty (SLT), offer a repeatable, minimally invasive treatment option. These lasers selectively target specific cells to improve fluid outflow without causing significant tissue damage.
- Micro-invasive Implants: Devices like the iStent inject, the smallest medical device ever approved by the FDA, can be implanted during cataract surgery. It helps fluid bypass the blocked drainage channels, thus lowering eye pressure.
- Sustained Drug Delivery Systems: These systems provide continuous medication delivery to the eye, eliminating the need for daily eye drops. Examples include drug-eluting implants and contact lenses.
- Telemedicine and Digital Monitoring: Advances in telemedicine and digital monitoring allow for remote patient monitoring, which is particularly useful for tracking disease progression and treatment adherence.
- AI and Machine Learning: Artificial intelligence (AI) and machine learning are being integrated into diagnostic processes. These technologies can analyze complex visual field data and imaging to assist in early detection and predict disease progression.
- Gene Therapy and Regenerative Medicine: Research in gene therapy and regenerative medicine is underway, aiming to repair or regenerate damaged optic nerve fibers, offering potential future treatments for glaucoma.
- Customized Treatment Approaches: Personalized medicine, based on individual genetic makeup, is becoming more prevalent, allowing for treatments tailored to the specific needs and responses of individual patients.
- Smart Eye Drops and Electronic Medication Dispensers: These technologies can remind patients to take their medication and monitor adherence, which is crucial for effective treatment.
These advancements represent significant steps forward in managing glaucoma and ocular hypertension, offering more effective, efficient, and patient-friendly treatment options. Ongoing research and innovation continue to expand the possibilities in treating these eye conditions.
Prevention Strategies
While it’s not always possible to prevent glaucoma or ocular hypertension, certain strategies can help reduce risk and detect these conditions early. Here are some key prevention strategies:
- Regular Eye Exams: Routine comprehensive eye examinations are the most effective way to detect glaucoma and ocular hypertension early. The frequency of eye exams should increase with age, especially for those at higher risk.
- Know Your Family History: Since glaucoma can be hereditary, knowing if family members have had it is important for assessing your risk.
- Exercise Regularly: Moderate, regular physical exercise may help lower eye pressure. However, certain high-intensity exercises and yoga positions that involve head-down postures may increase eye pressure and should be avoided.
- Maintain a Healthy Diet: A diet rich in fruits and vegetables, particularly dark, leafy greens, may have a beneficial effect on eye health.
- Protect Your Eyes: Eye injuries can lead to glaucoma. Wearing protective eyewear during sports or while engaging in activities involving potential eye hazards can help prevent such injuries.
- Use Eye Drops as Prescribed: If you are at risk for, or have been diagnosed with, ocular hypertension or glaucoma, it’s crucial to use any prescribed eye drops exactly as directed.
- Limit Caffeine: Excessive caffeine may increase eye pressure, so moderation is key.
- Stay Hydrated: Drinking fluids in moderation throughout the day can prevent spikes in eye pressure.
- Avoid Smoking: Smoking can harm eye health and increase the risk of glaucoma.
- Monitor Other Health Conditions: High blood pressure and diabetes, if not well-managed, can increase the risk of developing glaucoma.
- Wear Sunglasses: UV protection sunglasses can protect the eyes from harmful UV rays.
- Reduce Stress: While the link between stress and eye pressure is not clear, overall health benefits, including potentially those for eye health, are associated with stress reduction.
Implementing these strategies can contribute to better eye health and may help in the early detection and management of glaucoma and ocular hypertension. However, they are not a substitute for professional medical advice and regular eye exams.
Community and Support
Living with glaucoma or ocular hypertension can be challenging, but community and support resources play a vital role in helping individuals cope with their condition, manage treatment, and maintain their quality of life.
Here are some avenues for community and support:
- Support Groups: Many local and online support groups exist for people with glaucoma or ocular hypertension. These groups provide a platform to share experiences, coping strategies, and receive emotional support from others who understand the challenges of living with these conditions.
- Patient Education Programs: Hospitals, eye care centers, and health organizations often offer educational programs to help patients and their families understand the disease, its management, and lifestyle adaptations.
- Online Communities and Forums: Online platforms can be a great resource for connecting with others, accessing information, and finding encouragement. Websites of organizations like the Glaucoma Research Foundation or the American Glaucoma Society often host forums and community sections.
- Counseling Services: Professional counseling can help individuals cope with the emotional and psychological impact of a chronic condition like glaucoma, including dealing with anxiety or depression.
- Vision Rehabilitation Services: These services assist those who have experienced vision loss, providing training in using adaptive devices, mobility training, and strategies to perform daily activities.
- Educational Materials and Resources: Organizations dedicated to eye health often provide informative materials that can help patients understand their condition and treatment options better.
- Advocacy Groups: Groups like the Glaucoma Foundation and the National Glaucoma Research program advocate for research, improved treatments, and raise awareness about glaucoma and ocular hypertension.
- Social Services and Assistance: Social workers or local community health services can provide assistance with accessing medical care, transportation services, and other resources needed to manage glaucoma or ocular hypertension.
- Volunteer Opportunities: Getting involved in volunteer work related to glaucoma awareness and support can be empowering and provide a sense of purpose and community connection.
- Regular Updates from Eye Health Professionals: Staying in regular contact with eye care professionals and attending scheduled appointments is crucial. They can provide updates on new treatments, management strategies, and ongoing support.
Engaging with these resources can significantly alleviate the burden of living with glaucoma or ocular hypertension. It’s important for individuals to seek out support, stay informed, and remain proactive in managing their eye health.
Global Statistics and Research
Global statistics on glaucoma indicate its significant impact on vision health worldwide.
As of recent data:
- In the United States, over 120,000 people are blind from glaucoma, representing 9% to 12% of all cases of blindness. Glaucoma is the second leading cause of blindness globally and the leading cause of blindness among African Americans.
- The estimated global population affected by primary open-angle glaucoma (POAG) is approximately 68.56 million.
- Nearly 95 million people worldwide have glaucoma, with about 10 million blind in at least one eye. Many more suffer from visual impairment and impacts on daily living due to glaucoma. Current treatments do not restore vision lost from glaucoma, emphasizing the importance of early detection and effective treatment.
- Projections indicated that around 76 million people would suffer from glaucoma by 2020, with this number expected to reach 111.8 million by 2040.
Recent research in glaucoma treatment has identified new therapeutic targets. Researchers at Indiana University School of Medicine have discovered that restoring mitochondrial homeostasis in diseased neurons can protect optic nerve cells from damage. This finding is significant because glaucoma is a neurodegenerative disease that leads to vision loss and blindness due to optic nerve damage.
The study involved using induced pluripotent stem cells (iPSCs) from patients with and without glaucoma and CRISPR-engineered human embryonic stem cells with a glaucoma mutation. The research revealed that glaucomatous retinal ganglion cells suffer from mitochondrial deficiency, leading to mitochondrial damage and degeneration.
Enhancing mitochondrial biogenesis with a pharmacological agent could reverse this process. This approach aims to distribute the adenosine triphosphate production load among more mitochondria, thereby restoring the organelle’s physiology and potentially protecting the optic nerve.
These advancements and insights are crucial for developing more effective treatments and management strategies for glaucoma, which remains a leading cause of vision loss worldwide.
Similarities between Glaucoma and Ocular Hypertension
Glaucoma and Ocular Hypertension share several similarities, which are important in understanding their relationship and management:
- Elevated Intraocular Pressure (IOP): Both conditions are characterized by higher-than-normal pressure inside the eye. This is a key factor in the development and monitoring of both conditions.
- Asymptomatic Nature: Especially in their early stages, both glaucoma and ocular hypertension often present no symptoms. This means individuals may not realize they have either condition without regular eye examinations.
- Risk Factor for Glaucoma: Ocular hypertension is considered a significant risk factor for the development of glaucoma. Not everyone with ocular hypertension will develop glaucoma, but the elevated IOP increases the risk.
- Diagnostic Methods: Both conditions are primarily diagnosed through the measurement of intraocular pressure using tonometry during a comprehensive eye exam. Additional tests, such as visual field tests and examination of the optic nerve, are also important, particularly in diagnosing glaucoma.
- Management with Eye Drops or Medication: In cases where treatment is deemed necessary, both glaucoma and ocular hypertension can be managed with similar types of medications, often in the form of eye drops, which aim to lower intraocular pressure.
- Regular Monitoring: Both conditions require ongoing monitoring by an eye care professional. This includes regular checks of the intraocular pressure and the health of the optic nerve, especially important for individuals with ocular hypertension to monitor for the potential onset of glaucoma.
- Target Demographic: While anyone can develop either condition, they are more commonly observed in older adults, and certain demographic factors (like family history and ethnicity) can increase the risk for both.
Understanding these similarities is crucial for early detection and effective management of both ocular hypertension and glaucoma, to preserve vision and prevent potential complications.
Conclusion
Glaucoma and ocular hypertension are significant eye conditions that affect millions worldwide. Glaucoma, often linked to increased intraocular pressure, leads to optic nerve damage and can result in irreversible vision loss. Ocular hypertension, characterized by elevated eye pressure without associated nerve damage, is a major risk factor for developing glaucoma.
Both conditions often present without early symptoms, making regular eye exams crucial for early detection and management. Advances in medical research are continuously improving treatment options, focusing on pressure management and nerve protection. Effective management of these conditions involves a combination of medical treatment, regular monitoring, and lifestyle adjustments, emphasizing the importance of early detection and ongoing care.