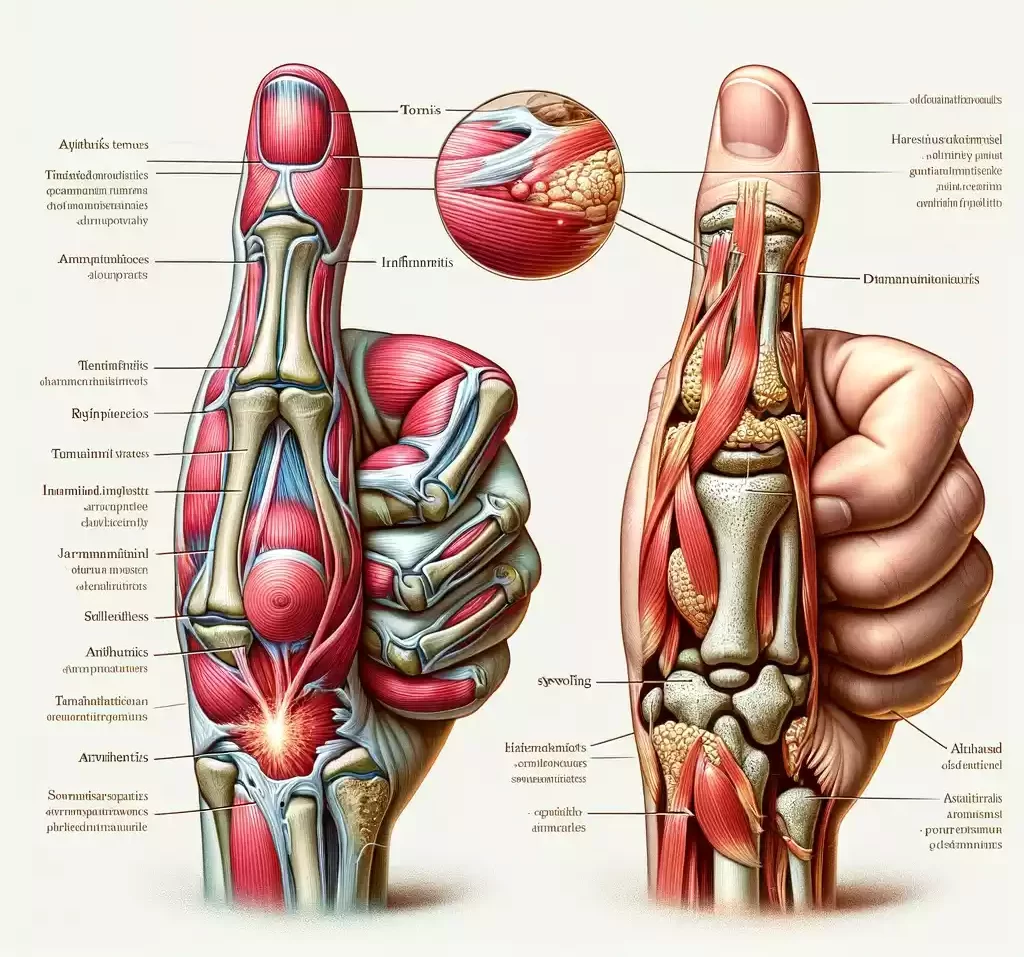
Tendonitis and Arthritis in the thumb are two distinct but often related conditions affecting the thumb joint. Tendonitis, specifically in the thumb, typically refers to the inflammation of the tendons – the cords that attach muscle to bone – which can cause pain and tenderness along the thumb side of the wrist, especially when gripping or pinching. Arthritis in the thumb, on the other hand, usually pertains to osteoarthritis, a degenerative joint disease where the cartilage covering the ends of bones wears away, leading to pain, swelling, and decreased mobility in the thumb joint. Both conditions can significantly impact hand function and daily activities.
Tendonitis
Tendonitis, also spelled tendinitis, is a medical condition characterized by the inflammation or irritation of a tendon. Tendons are the strong, fibrous cords that attach muscles to bones. This inflammation typically results in pain, tenderness, and sometimes swelling near a joint. Tendonitis commonly occurs from repetitive strain or overuse of a tendon during activities, but it can also develop due to age-related wear and tear.

The condition can affect tendons in various parts of the body, including the shoulder, elbow, wrist, knee, and heel. Treatment typically involves rest, ice, and over-the-counter anti-inflammatory medications, with more severe cases potentially requiring physical therapy or other medical interventions.
Causes of Tendonitis
Tendonitis is caused by the inflammation of a tendon, and it usually results from a combination of overuse and strain. The most common causes include:
- Repetitive Motion: Frequent and repetitive use of a tendon, especially during certain jobs, sports, or daily activities, can lead to overuse and strain.
- Sudden Injury: Acute injuries, often occurring during sports or sudden movements, can cause tendonitis.
- Age: As people age, their tendons become less flexible and more prone to injury, making older adults more susceptible to tendonitis.
- Poor Technique or Ergonomics: Incorrect technique in sports or work-related activities can put unnecessary stress on tendons.
- Medical Conditions: Certain conditions, such as rheumatoid arthritis or diabetes, can increase the risk of developing tendonitis.
- Physical Stress: Excessive physical exertion or carrying heavy loads can stress the tendons.
Symptoms of Tendonitis
The symptoms of tendonitis can vary depending on the affected tendon, but commonly include:
- Pain: The hallmark symptom of tendonitis, often described as a dull ache, particularly when moving the affected limb or joint.
- Tenderness: The area around the inflamed tendon is usually tender to the touch.
- Mild Swelling: There may be slight swelling in the area around the tendon.
- Stiffness: The affected joint might feel stiff, especially after periods of inactivity or in the morning.
- Warmth and Redness: The skin over the affected tendon may become warm and appear red due to inflammation.
- Restricted Movement: Movements involving the tendon can become difficult or painful.
- A Grating or Cracking Sensation: Some people experience a sensation of grating or cracking when the tendon is moved. This condition, known as crepitus, is due to the tendon rubbing against surrounding tissues.
Arthritis in Thumb
Arthritis in the thumb, often specifically referring to osteoarthritis, is a condition characterized by the degeneration and breakdown of cartilage in the thumb joint. This joint, known as the carpometacarpal (CMC) joint, is where the thumb meets the wrist. As the cartilage, which normally cushions the joint, wears away, it leads to pain, swelling, stiffness, and a decrease in mobility in the thumb.

Symptoms of thumb arthritis can include pain during activities that involve gripping or pinching, swelling and tenderness at the base of the thumb, decreased strength when grasping or pinching objects, and an enlarged or bony appearance of the joint.
The condition is more common with aging and can be exacerbated by repetitive stress on the joint. Treatment options for thumb arthritis range from non-surgical interventions like splinting, anti-inflammatory medications, and corticosteroid injections to surgical procedures in more advanced cases.
Causes of Arthritis in Thumb
Arthritis in the thumb, particularly at the carpometacarpal (CMC) joint, can be caused by several factors:
- Age-Related Wear and Tear: The most common cause of thumb arthritis is the natural wear and tear of the joint that occurs with aging. Over time, the cartilage that cushions the bones wears away, leading to arthritis.
- Repetitive Stress: Activities or jobs that involve repetitive hand motions, particularly those that put stress on the thumb, can contribute to the development of arthritis.
- Injury or Trauma: Past injuries to the thumb joint, such as fractures or sprains, can increase the risk of developing arthritis in that joint later in life.
- Genetic Factors: There may be a genetic predisposition to developing arthritis, meaning it can sometimes run in families.
- Inflammatory Diseases: Conditions like rheumatoid arthritis, which causes inflammation of the joints, can also affect the thumb.
- Sex: Women are more likely than men to develop thumb arthritis, possibly due to differences in joint anatomy and hormonal influences.
Symptoms of Arthritis in Thumb
The symptoms of arthritis in the thumb, especially osteoarthritis in the carpometacarpal (CMC) joint, typically include:
- Pain: This is the most common symptom, often felt at the base of the thumb. The pain may be particularly noticeable during activities that involve gripping, pinching, or applying force with the thumb, such as opening jars, turning keys, or writing.
- Swelling and Stiffness: The thumb base may become swollen and stiff. Stiffness can be more pronounced in the morning or after periods of inactivity.
- Decreased Strength and Range of Motion: As the condition progresses, you might experience a decrease in the strength of your grip or pinch and difficulty performing tasks that require these actions.
- Enlarged Joint Appearance: The joint at the base of the thumb may appear enlarged or develop a bony prominence due to bone changes and swelling.
- Grinding Sensation: Some people feel a grinding or catching sensation (crepitus) when moving the thumb, caused by the roughened surfaces of the bones rubbing together.
- Tenderness to the Touch: The area might be tender when you press on it.
- Decreased Pinch and Grip Ability: Difficulty with tasks that require pinching, such as picking up small objects, can be a significant symptom.
- Changes in Thumb Shape: In advanced cases, there might be noticeable changes in the shape of the thumb due to joint deterioration and bone movement.
Importance of understanding the difference between Tendonitis and Arthritis in Thumb
Understanding the difference between tendonitis and arthritis in the thumb is crucial for several reasons:
- Accurate Diagnosis: Differentiating between the two conditions is key to an accurate diagnosis. Misdiagnosis can lead to ineffective treatment and prolonged discomfort.
- Appropriate Treatment: Each condition requires a specific treatment approach. For instance, tendonitis may respond well to rest and physical therapy, while arthritis might need more long-term management strategies like joint protection techniques and possibly surgery.
- Prevention of Further Injury: Knowing the exact condition helps in implementing preventive measures. In tendonitis, modifying activities to reduce strain on the tendon is essential, while in arthritis, protecting the joint from further wear and tear is crucial.
- Management of Expectations: Understanding the nature of the condition helps in setting realistic expectations regarding recovery time, treatment effectiveness, and the possibility of recurrence or progression.
- Lifestyle Adjustments: Each condition may require different adjustments in daily activities or work tasks to manage symptoms and prevent exacerbation.
- Understanding Long-Term Implications: Tendonitis often has a shorter duration and may resolve with appropriate treatment, whereas arthritis is a chronic condition that typically progresses over time and requires ongoing management.
- Educational Purposes: Educating patients about their condition empowers them to take an active role in their treatment and understand the importance of adhering to therapeutic regimes and lifestyle modifications.
Distinguishing between tendonitis and arthritis in the thumb ensures that patients receive the correct treatment, understand their condition better, and are able to manage their symptoms effectively, leading to better outcomes and quality of life.
Comparison table of Tendonitis and Arthritis in Thumb
Here’s a comparison table outlining the key differences between Tendonitis and Arthritis in the Thumb:
| Feature | Tendonitis | Arthritis in Thumb (Osteoarthritis) |
|---|---|---|
| Definition | Inflammation of the tendon, often due to overuse or repetitive strain. | Degeneration of cartilage in the thumb joint leads to pain and joint dysfunction. |
| Primary Cause | Overuse, repetitive motion, sudden injury, or strain. | Age-related wear and tear, repetitive stress, injury, genetic factors. |
| Common Location | Any tendon, but in the context of the thumb, it typically affects the tendons around the wrist. | The carpometacarpal (CMC) Joint is located in the middle of thumb. |
| Symptoms | Pain, tenderness, mild swelling, restricted movement, stiffness, warmth, and sometimes redness. | Pain, swelling, stiffness, decreased strength and range of motion, grinding sensation, and joint enlargement. |
| Onset | Can be sudden after intense activity, or gradual due to repetitive strain. | Gradual, often developing over the years. |
| Aggravating Activities | Activities that involve the repetitive movement of the affected tendon. | Activities involving gripping, pinching, or twisting movements of the thumb. |
| Treatment | Rest, ice, anti-inflammatory medications, physical therapy, avoiding repetitive strain. | Splinting, anti-inflammatory medications, physical therapy, corticosteroid injections, surgery in severe cases. |
| Age Group Commonly Affected | All ages, but more common in adults engaged in repetitive activities or certain sports. | Typically older adults, are more common after the age of 50. |
| Progression | Usually resolves with proper treatment and rest. May become chronic if not addressed. | Generally progressive; symptoms may worsen over time without treatment. |
Understanding these differences can be crucial for proper diagnosis and treatment. If you suspect you have tendonitis or arthritis in your thumb, it is important to consult a healthcare professional for an accurate diagnosis and appropriate treatment plan.
Diagnosis Approaches of Tendonitis and Arthritis in Thumb
The diagnosis of tendonitis and arthritis in the thumb involves different approaches, as they are distinct conditions:
Tendonitis
- Medical History and Physical Examination: The doctor will discuss your symptoms, activities that may have caused them, and any previous injuries. A physical exam to check for pain, swelling, and range of motion in the thumb is essential.
- Imaging Tests:
- X-rays: Although they can’t visualize tendons, X-rays can rule out other causes of thumb pain, such as arthritis or fractures.
- Ultrasound or MRI: These imaging tests can provide detailed images of the soft tissues, including tendons, and may be used if the diagnosis is unclear.
- Functional Tests: These may be performed to assess the impact of the condition on movement and strength.
Arthritis in the Thumb
- Medical History and Physical Examination: This includes discussing the patient’s symptoms, duration, and any activities that exacerbate pain. The doctor will examine the thumb for swelling, pain, range of motion, and signs of joint changes.
- Imaging Tests:
- X-rays: Essential for diagnosing thumb arthritis, X-rays can show joint space narrowing, changes in bone, and the formation of bone spurs.
- MRI or CT scans: These are less commonly used but can provide more detailed images of the joint and surrounding tissues.
- Joint Function Tests: To assess the extent to which arthritis has affected the joint’s functionality.
Treatment option for Tendonitis and Arthritis in Thumb

The treatment options for tendonitis and arthritis in the thumb are tailored to the specific condition, severity, and individual needs:
Tendonitis
- Rest: Avoid activities that exacerbate the pain to allow the tendon to heal.
- Ice Therapy: Applying ice packs to the affected area can help reduce inflammation and pain.
- Over-the-Counter Pain Relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can reduce pain and swelling.
- Bracing or Splinting: A brace or splint can immobilize the thumb and wrist, allowing the tendon to rest and heal.
- Physical Therapy: Exercises to strengthen and stretch the affected tendon and surrounding muscles can be beneficial.
- Corticosteroid Injections: Injections may be used for severe pain and inflammation but are generally used sparingly.
- Surgery: In rare cases, if the tendonitis is severe and does not respond to other treatments, surgery may be considered.
Arthritis in Thumb
- Pain Management: NSAIDs or acetaminophen can be used to manage pain and inflammation.
- Splinting: Wearing a splint can help support the joint, reduce pain, and prevent further deformity.
- Heat and Cold Therapy: Applying heat can help relax and loosen tissues, while cold can reduce inflammation and numb sore areas.
- Physical and Occupational Therapy: These therapies can help improve joint function, reduce pain, and suggest modifications to reduce stress on the joint.
- Corticosteroid Injections: Provides temporary relief for inflammation and pain.
- Surgery: If conservative treatments fail and the arthritis is severe, options like joint fusion (arthrodesis) or joint replacement might be considered.
It’s essential to consult with a healthcare professional for an accurate diagnosis and to determine the most appropriate treatment plan for your specific condition. Treatment plans can vary greatly depending on individual circumstances, including the severity of the condition, lifestyle, and overall health.
Physical Therapy and Exercises
Physical therapy and exercises are vital components in the management and rehabilitation of various musculoskeletal conditions, including tendonitis and arthritis in the thumb.

Here’s an overview of how physical therapy and specific exercises can help:
For Tendonitis
- Stretching Exercises: Gentle stretching helps maintain flexibility and range of motion in the affected tendon and surrounding muscles. For thumb tendonitis, this might include wrist and thumb stretches.
- Strengthening Exercises: Once pain subsides, gradual strengthening exercises are introduced to build up the muscles around the affected tendon, providing better support and reducing the risk of future injury.
- Ergonomic and Technique Adjustments: Physical therapists often advise on modifying activities or ergonomic setups that may have contributed to tendonitis, reducing strain on the affected tendon.
- Manual Therapy: Therapists may use techniques like massage or mobilization to improve movement and reduce pain.
- Ultrasound or Heat Therapy: These modalities can be used to promote healing and reduce pain.
For Arthritis in Thumb
- Range of Motion Exercises: Gentle exercises to keep the thumb joint flexible and to maintain as much function as possible.
- Strengthening Exercises: Focus on strengthening the muscles around the thumb to improve joint stability and function. This might include exercises using resistance bands or light hand weights.
- Joint Protection Strategies: Learning how to protect the thumb joint during daily activities to reduce pain and prevent further joint damage.
- Heat Therapy: Applying heat can help reduce stiffness and improve comfort, especially before exercise.
- Assistive Devices Training: Occupational therapists may recommend splints or other assistive devices to support the joint and reduce pain during activities.
General Tips
- Start Slowly: Begin with gentle exercises and gradually increase intensity under guidance.
- Consistency: Regular exercise is key to improving symptoms.
- Pain Management: Be mindful of pain levels; exercises should not exacerbate pain significantly.
- Professional Guidance: It’s important to work with a physical or occupational therapist for tailored exercises and advice.
Effective physical therapy and exercises can significantly improve symptoms, enhance quality of life, and help in managing both tendonitis and arthritis in the thumb. Always consult a physician before starting any new exercise program.
Recent Advances and Research
There are Recent research and advances in the treatment of tendonitis and arthritis:
Recent Advances in Tendonitis Treatment
- Regenerative Medicine Techniques: Recent research in tendonitis treatment has increasingly focused on regenerative medicine, including platelet-rich plasma (PRP) therapy and stem cell therapy. These approaches aim to enhance the body’s natural healing processes.
- Improved Physical Therapy Techniques: There’s ongoing development in physical therapy, focusing on more targeted exercises and therapies that can accelerate recovery and reduce the risk of recurrence.
- Advancements in Surgical Techniques: For severe cases of tendonitis that do not respond to conservative treatment, advancements in minimally invasive surgical techniques can provide better outcomes with shorter recovery times.
- Use of Biologics: The use of biologics, such as growth factors and cytokines, is an area of exploration for enhancing tendon healing.
- Ultrasound-Guided Treatments: The use of ultrasound in diagnosis and treatment, including guiding injections and assessing the healing process, has become more refined.
Recent Advances in Arthritis Treatment
- New Mechanisms and Drug Targets: Recent research has uncovered new molecular mechanisms behind arthritis, such as the role of specific proteins and genetic factors, opening the door to targeted drug therapies.
- Cartilage Tissue Engineering: Advances in tissue engineering hold promise for developing new ways to repair or regenerate deteriorated cartilage in arthritic joints.
- Biologic Therapies: Biologic drugs, which target specific parts of the immune system, have become more sophisticated, offering new treatment avenues for inflammatory types of arthritis.
- Personalized Medicine: There’s a growing emphasis on personalized medicine in arthritis treatment, focusing on tailoring treatments to individual patient profiles, including genetic, environmental, and lifestyle factors.
- Wearable Technology: The use of wearable technology for monitoring symptoms and progression of arthritis, as well as adherence to treatment protocols, is becoming more common.
Similarities between Tendonitis and Arthritis in Thumb
Tendonitis and arthritis in the thumb, despite being distinct conditions, share several similarities:
- Pain in the Thumb Area: Both conditions commonly cause pain in the thumb, especially during activities that involve movement or pressure in the area.
- Swelling and Stiffness: Both can lead to swelling and stiffness in the thumb, contributing to a reduced range of motion and discomfort.
- Aggravated by Certain Activities: Activities that involve repetitive thumb movements or stress on the thumb joint, like gripping, pinching, or twisting, can exacerbate symptoms in both conditions.
- Common in Older Adults: While tendonitis can occur at any age, it, like arthritis, is more commonly seen in older adults due to wear and tear and reduced healing capacity.
- Can Affect Daily Activities: Both conditions can impact daily activities, particularly those requiring fine motor skills, grip strength, or manual dexterity.
- Management Strategies: Initial treatment strategies for both conditions may include rest, ice, and the use of over-the-counter pain relievers or anti-inflammatory medications.
- Physical Therapy and Exercises: Both conditions may benefit from physical therapy and specific exercises aimed at improving strength and flexibility in the thumb and wrist area.
- Need for Medical Intervention in Severe Cases: In severe cases, both tendonitis and arthritis might require more advanced medical interventions, which can include corticosteroid injections or even surgery.
Conclusion
Tendonitis and Arthritis in the thumb are two distinct conditions that both affect the thumb joint but have different underlying causes and treatment approaches. Tendonitis involves inflammation of the tendons, usually due to overuse or strain, and is characterized by pain, swelling, and stiffness, often resolving with rest, physical therapy, and anti-inflammatory treatments.
Arthritis, particularly osteoarthritis in the thumb, results from the degeneration of joint cartilage, leading to chronic pain, swelling, and reduced mobility, requiring a more long-term management strategy that may include medication, lifestyle adjustments, and possibly surgery. Understanding the differences between these conditions is essential for accurate diagnosis, effective treatment, and optimal management of thumb joint health.