Corneal Dystrophy and Degeneration encompass a group of eye conditions characterized by the gradual breakdown or abnormal changes in the cornea, the transparent front part of the eye. These conditions often lead to impaired vision due to the accumulation of cloudy or opaque material within the cornea, affecting its clarity and transparency. Corneal dystrophies are typically inherited, while degenerations can result from various factors such as aging, trauma, or underlying health issues.
Symptoms may include blurry vision, light sensitivity, discomfort, or distorted vision. Management approaches vary depending on the specific type and severity, ranging from prescription eyeglasses to more advanced treatments like corneal transplants or therapeutic interventions to alleviate symptoms and preserve vision. Regular eye examinations are crucial for early detection and appropriate management of these conditions.
What is Corneal Dystrophy?
Corneal dystrophy is a group of genetic eye disorders characterized by the gradual accumulation of abnormal substances or changes in the layers of the cornea—the clear, dome-shaped surface covering the front of the eye. These conditions are typically hereditary and lead to the buildup of cloudy or opaque material within the cornea, affecting its transparency and potentially causing vision problems.
Corneal dystrophies can impact different layers of the cornea and are categorized based on their location and the specific abnormalities they cause. They may lead to symptoms such as blurred vision, discomfort, recurrent corneal erosions, or in severe cases, vision loss.
Management approaches vary depending on the type and severity of the dystrophy and may include prescription eyeglasses, contact lenses, medications, corneal surgeries, or other specialized treatments to maintain eye health and visual clarity. Regular eye examinations are essential for early detection and appropriate management of corneal dystrophies.
Causes
Here are the primary causes associated with corneal dystrophies:
- Genetic Factors: Most corneal dystrophies are inherited, passed down through generations due to genetic mutations affecting proteins in the cornea.
- Abnormal Protein Accumulation: Genetic mutations can lead to the abnormal accumulation of various proteins within the cornea, disrupting its normal structure and function.
- Age-related Changes: Some corneal dystrophies may exhibit age-related degenerative changes, causing gradual alterations in the corneal tissues over time.
- Metabolic Disorders: Certain metabolic conditions or systemic diseases can contribute to the development or progression of corneal dystrophies.
- Environmental Factors: While less common, environmental influences or external factors could potentially impact the progression or severity of certain corneal dystrophies.
Symptoms
Corneal dystrophies can manifest differently based on the specific type and stage of the condition. Some common symptoms associated with various corneal dystrophies include:
- Blurred Vision: Gradual blurring of vision is a typical symptom due to the accumulation of abnormal substances or changes in the corneal layers, impacting its transparency.
- Recurrent Corneal Erosions: Some dystrophies may cause the outer layer of the cornea to weaken, leading to recurrent corneal erosions. This can result in pain, discomfort, and a sensation of a foreign body in the eye.
- Sensitivity to Light: Increased sensitivity to light (photophobia) might occur, making it uncomfortable to be in well-lit environments.
- Reduced Visual Clarity: The presence of cloudy or opaque areas within the cornea can reduce visual clarity, affecting both near and distant vision.
- Distorted Vision: Vision may appear distorted or wavy due to irregularities in the cornea caused by the dystrophy.
- Eye Irritation or Discomfort: Some individuals may experience eye irritation, a gritty sensation, or mild to moderate eye discomfort.
- Visual Halos or Glare: Seeing halos around lights or experiencing glare, particularly in low-light conditions, can be a symptom associated with certain corneal dystrophies.
What is Corneal Degeneration?
Corneal degeneration refers to a group of non-inflammatory eye conditions characterized by structural changes, abnormalities, or degenerative alterations in the cornea—the transparent, dome-shaped outer layer of the eye. Unlike corneal dystrophies, which are primarily genetic and involve the gradual accumulation of abnormal material within the cornea, degenerations can result from various factors such as aging, trauma, systemic diseases, environmental factors, or metabolic disorders.
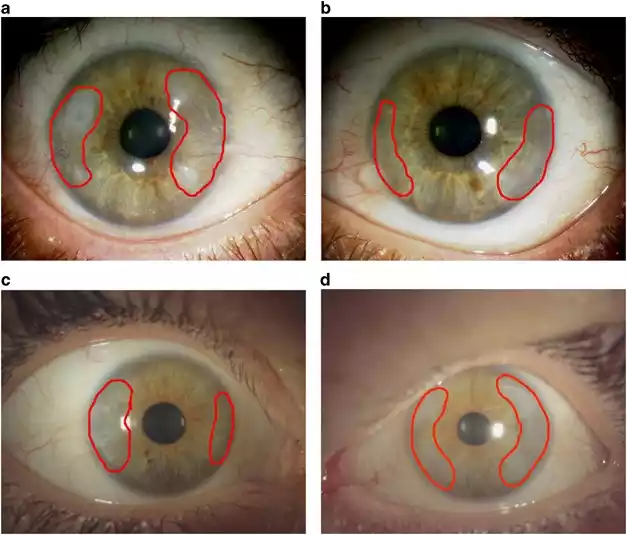
These degenerative changes often lead to modifications in the cornea’s structure, impacting its clarity and functionality. Corneal degenerations encompass a range of conditions, including but not limited to keratoconus (a progressive thinning and bulging of the cornea), Salzmann’s nodular degeneration (formation of elevated nodules on the corneal surface), or band-shaped keratopathy (deposition of calcium in the cornea).
Symptoms of corneal degenerations can vary depending on the specific condition but commonly include blurry or distorted vision, sensitivity to light, discomfort, or, in severe cases, vision impairment.
Management of corneal degenerations aims to address symptoms and may involve the use of corrective lenses, specialized contact lenses, corneal collagen cross-linking (used in keratoconus), or, in advanced cases, surgical interventions such as corneal transplantation. Regular monitoring by an eye care professional is essential to manage these conditions effectively and preserve visual function.
Causes
Here are the primary causes associated with corneal degeneration:
- Aging: Natural aging processes can lead to structural changes in the cornea over time, contributing to degenerative conditions.
- Genetic Factors: Some corneal degenerations can have a genetic predisposition, making individuals more susceptible to developing these conditions.
- Trauma or Injury: Previous eye injuries or trauma to the cornea can sometimes result in degenerative changes, impacting its structure and function.
- Environmental Factors: Prolonged exposure to ultraviolet (UV) radiation, certain chemicals, or environmental toxins can potentially contribute to corneal degeneration.
- Systemic Diseases: Underlying systemic conditions such as certain autoimmune diseases or metabolic disorders may play a role in the development or progression of corneal degenerations.
- Other Factors: Certain lifestyle habits, chronic eye irritation, or prolonged use of contact lenses might also influence the onset or severity of some corneal degenerative conditions.
Symptoms
The symptoms of corneal degeneration can vary based on the specific type of degeneration and its severity. Some common symptoms include:
- Blurry or Distorted Vision: Visual disturbances may occur, making objects appear blurry, hazy, or distorted.
- Recurrent Changes in Prescription: Frequent changes in eyeglass or contact lens prescription due to fluctuations in vision quality.
- Increased Sensitivity to Light: Photophobia or heightened sensitivity to light sources, leading to discomfort or squinting in bright environments.
- Irregular Astigmatism: Corneal irregularities may cause astigmatism, resulting in distorted or ghosted images.
- Eye Discomfort or Pain: Some individuals may experience eye irritation, foreign body sensation, or occasional mild to moderate pain.
- Halos or Glare: Seeing halos around lights or experiencing glare, particularly at night or in low-light conditions.
- Decreased Visual Acuity: Gradual decline in visual clarity or acuity, affecting overall vision quality.
Comparison table of Corneal Dystrophy and Degeneration
Here’s a comparison table outlining the key differences between Corneal Dystrophy and Corneal Degeneration:
| Aspect | Corneal Dystrophy | Corneal Degeneration |
|---|---|---|
| Cause | Primarily genetic inheritance | Various factors like aging, trauma, environment |
| Inheritance | Often inherited (autosomal dominant/recessive) | Not primarily inherited, can be multifactorial |
| Onset | Typically manifests in childhood/adulthood | Can occur at any age, not limited to specific age |
| Progression | Slow and gradual progression over time | Variable progression rate depending on the condition |
| Underlying Changes | Abnormal substance accumulation within cornea | Structural changes, irregularities in corneal layers |
| Types | Various types affecting different corneal layers | Different types based on distinct corneal alterations |
| Symptoms | Blurred vision, recurrent erosions, discomfort | Blurry vision, distorted vision, discomfort |
| Treatment | Management focuses on symptom alleviation | Treatment aims to address symptoms, slow progression |
| Examples | Epithelial basement membrane dystrophy, Stromal/Endothelial dystrophies | Keratoconus, Salzmann’s nodular degeneration, etc. |
This table provides a simplified comparison highlighting the fundamental differences between corneal dystrophies and corneal degenerations, emphasizing their causes, characteristics, progression, and treatment approaches. Each condition within these categories can have specific nuances and subtypes, so professional evaluation is crucial for accurate diagnosis and tailored treatment plans.
What are the similarities between Corneal Dystrophy and Degeneration?
While corneal dystrophy and corneal degeneration are distinct conditions with differing causes and characteristics, they do share certain similarities:
- Corneal Impact: Both conditions affect the cornea, the transparent outer layer of the eye, leading to alterations in its structure, which can result in impaired vision.
- Visual Symptoms: Both corneal dystrophies and degenerations can cause visual disturbances, such as blurry vision, distorted vision, and decreased visual acuity.
- Potential Vision Complications: Both conditions, if left untreated or unmanaged, can lead to more severe vision complications or vision loss over time.
- Management and Treatment: Treatment approaches for both corneal dystrophy and corneal degeneration focus on managing symptoms, preserving vision, and slowing down the progression of the condition. Treatment methods might involve prescription eyeglasses, contact lenses, medications, and in more advanced cases, surgical interventions like corneal transplantation.
- Ophthalmologic Evaluation: Diagnosis of both conditions requires a comprehensive eye examination by an ophthalmologist or corneal specialist, often involving tests such as corneal topography, slit-lamp examination, or other specialized assessments to determine the specific condition and its severity.
- Impact on Daily Life: Both corneal dystrophies and degenerations can affect an individual’s quality of life due to visual disturbances, discomfort, or the need for ongoing management and care.
Diagnosis of Corneal Dystrophy and Degeneration
Diagnosing corneal dystrophy and degeneration involves a comprehensive eye examination by an ophthalmologist or corneal specialist.

Here are the common diagnostic steps:
Medical History: The doctor will inquire about your symptoms, family history of eye conditions, past eye surgeries or injuries, and any underlying health conditions.
Visual Acuity Test: This standard eye test measures how well you see at various distances using an eye chart.
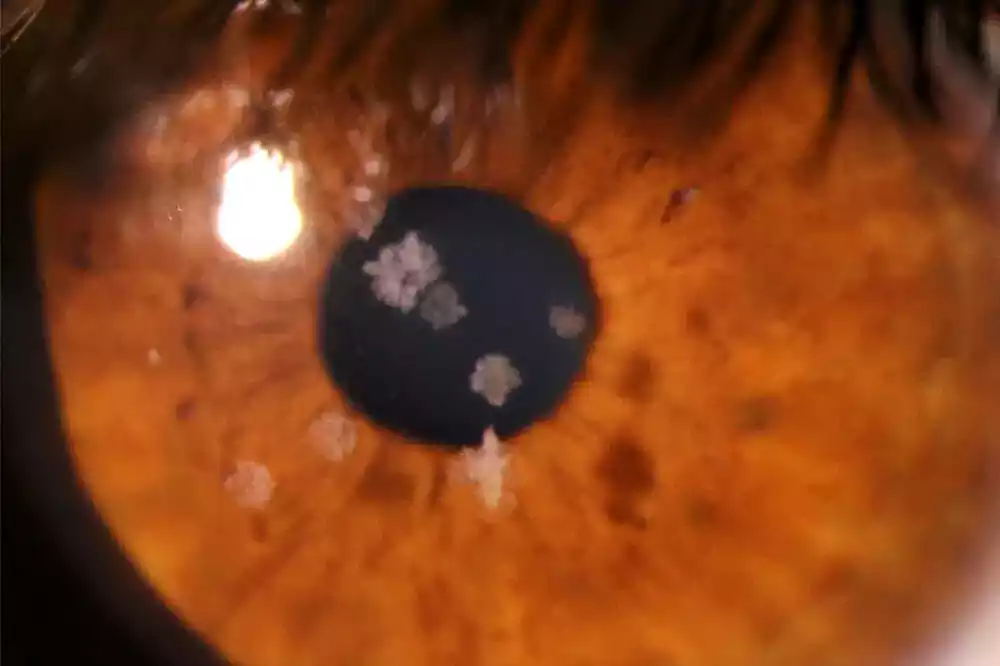
Slit-lamp Examination: A specialized microscope called a slit lamp allows the doctor to examine the cornea in detail. They’ll assess its transparency, look for abnormal deposits or changes, and evaluate the layers of the cornea.
Corneal Topography: This non-invasive test maps the curvature and shape of the cornea, aiding in the diagnosis of conditions like keratoconus by detecting irregularities.
Tear Film Assessment: Evaluation of tear film quality and quantity to assess if dry eye symptoms contribute to the condition.
Pachymetry: Measures the thickness of the cornea, which can be helpful in diagnosing conditions like Fuchs’ endothelial corneal dystrophy.
Genetic Testing (for Dystrophies): In cases suspected to be genetic dystrophies, genetic testing may be recommended to identify specific genetic mutations associated with certain dystrophies.
In Vivo Confocal Microscopy: This imaging technique allows for high-resolution imaging of corneal cells and structures, aiding in the diagnosis and monitoring of corneal dystrophies.
Biopsy or Additional Tests: In some complex cases, a corneal biopsy or other specialized tests may be necessary for a definitive diagnosis.
Treatment Approaches for Corneal Dystrophy and Degeneration
The treatment approaches for corneal dystrophy and degeneration aim to manage symptoms, preserve vision, and, in some cases, slow down the progression of the condition.
Here are the treatment options commonly used for both conditions:
Corneal Dystrophy:
- Medications: Lubricating eye drops or ointments can help alleviate discomfort and manage dryness associated with some types of corneal dystrophies.
- Contact Lenses: Specialized contact lenses, such as rigid gas permeable (RGP) or scleral lenses, may improve vision by providing a smoother surface for light to enter the eye, especially in cases of irregular corneal surfaces.
- Phototherapeutic Keratectomy (PTK): This laser procedure removes abnormal tissue or deposits from the cornea’s surface, improving vision in some types of corneal dystrophies.
- Corneal Transplantation: In advanced cases where vision is significantly affected, a corneal transplant (keratoplasty) might be necessary to replace the damaged corneal tissue with healthy donor tissue.
- New Therapies: Emerging treatments like gene therapy or targeted medications are being explored for certain types of corneal dystrophies, although they may still be in experimental stages.
Corneal Degeneration:
- Corrective Lenses: Eyeglasses or contact lenses may help correct vision issues caused by corneal irregularities in degenerative conditions like keratoconus.
- Corneal Collagen Cross-Linking (CXL): This procedure involves the application of riboflavin (vitamin B2) eye drops and UV light to strengthen corneal collagen fibers, slowing or halting the progression of keratoconus.
- Intacs Inserts: These small plastic inserts implanted into the cornea can help reshape it, improving vision in some cases of keratoconus.
- Corneal Transplant: In advanced stages of corneal degeneration where vision is severely affected and other treatments are ineffective, a corneal transplant may be recommended.
- Intrastromal Corneal Rings: Another surgical option for keratoconus involves inserting small plastic rings into the cornea to improve its shape and visual acuity.
The specific treatment approach depends on the type and severity of the condition, as well as the individual’s unique circumstances. Regular monitoring by an eye care professional is essential to assess the progression of the condition and determine the most suitable treatment plan to maintain eye health and visual function.
Impact on Vision and Daily Life
Both corneal dystrophies and degenerations can significantly impact vision and daily life due to their effects on the cornea, leading to various visual disturbances and discomfort.

Here’s how they can affect vision and daily activities:
Corneal Dystrophy:
- Blurred Vision: Accumulation of abnormal substances within the cornea can lead to blurred or cloudy vision, affecting both near and distant vision.
- Recurrent Corneal Erosions: Some dystrophies cause the cornea’s surface to become irregular, leading to recurrent corneal erosions. This can result in sudden episodes of pain, discomfort, and sensitivity to light.
- Visual Disturbances: Depending on the specific dystrophy and its severity, individuals may experience distorted vision, halos around lights, glare, or fluctuations in vision quality.
- Impact on Daily Life: Corneal dystrophies can affect various aspects of daily life, including difficulties in reading, driving, or performing tasks that require clear vision. Discomfort from recurrent erosions may affect overall quality of life.
Corneal Degeneration:
- Visual Disturbances: Conditions like keratoconus, Salzmann’s nodular degeneration, or band-shaped keratopathy can cause distorted or blurred vision, leading to difficulties in seeing clearly.
- Irregular Astigmatism: Keratoconus, in particular, can result in irregular astigmatism, making it challenging to correct vision with standard eyeglasses or contact lenses.
- Sensitivity to Light: Increased sensitivity to light (photophobia) is common in many corneal degenerations, making it uncomfortable to be in brightly lit environments.
- Impact on Daily Activities: Corneal degenerations can interfere with daily activities such as reading, driving, or using electronic devices due to visual disturbances and discomfort.
Preventive Measures
Preventive measures for corneal dystrophy and degeneration primarily focus on minimizing risk factors that could exacerbate these conditions or slow down their progression. While these conditions are often genetic or age-related, there are certain measures individuals can take to potentially reduce the risk or delay the progression:
- Regular Eye Exams: Routine eye examinations by an ophthalmologist or optometrist are crucial for early detection and timely management of any changes in the cornea. Detecting these conditions early can help implement appropriate interventions.
- Eye Protection: Wear protective eyewear, such as safety goggles or glasses, during activities that pose a risk of eye injury or trauma. This can help prevent damage that might contribute to the development or worsening of corneal conditions.
- Healthy Lifestyle: Maintaining overall health through a balanced diet rich in nutrients, regular exercise, and managing systemic conditions such as diabetes can indirectly support eye health.
- Proper Contact Lens Care: If you wear contact lenses, follow proper hygiene and care guidelines provided by your eye care professional. Improper lens care can increase the risk of corneal infections or complications.
- UV Protection: Use sunglasses that provide UV protection when outdoors. UV exposure can potentially impact the cornea’s health, so protecting your eyes from harmful UV rays is essential.
- Avoid Rubbing Eyes: Minimize rubbing or touching your eyes excessively, as this can irritate the cornea and potentially contribute to corneal erosions.
- Regular Follow-ups: For individuals diagnosed with corneal dystrophy or degeneration, consistent follow-ups with an eye care professional are critical. These visits can help monitor changes in the cornea and ensure appropriate management.
While these preventive measures may help reduce certain risk factors associated with corneal conditions, they may not entirely prevent the development or progression of genetic or age-related corneal issues. Individualized care and guidance from an eye care professional are crucial in managing these conditions effectively.
Research and Innovations
Research and innovation in the field of corneal dystrophy and degeneration focus on several areas aimed at better understanding these conditions, developing improved treatment options, and enhancing patient outcomes.
Here are some notable areas of ongoing research and innovations:
Genetic Studies: Researchers are delving deeper into the genetic underpinnings of various corneal dystrophies, identifying specific gene mutations associated with different types. This knowledge aids in early detection, genetic counseling, and potential gene therapies.
Advanced Imaging Techniques: Continued advancements in imaging technologies, such as optical coherence tomography (OCT) and in vivo confocal microscopy, provide detailed images of corneal structures, aiding in early diagnosis and monitoring disease progression.
Targeted Therapies: Investigating targeted medications or molecular therapies to inhibit the progression of corneal dystrophies by targeting specific pathways involved in the accumulation of abnormal substances within the cornea.
Gene Therapy: Exploring gene-based therapies to address underlying genetic mutations causing certain corneal dystrophies. Gene editing techniques and gene delivery systems are under investigation for potential treatments.
Tissue Engineering and Biomaterials: Research involves the development of artificial corneal implants, tissue-engineered corneas, or biocompatible materials to replace damaged corneal tissue, providing potential alternatives to traditional corneal transplants.
Corneal Cross-Linking: Continued research focuses on optimizing corneal collagen cross-linking (CXL) techniques for treating corneal degenerations like keratoconus. This includes refining protocols, studying combination therapies, and evaluating long-term outcomes.
Stem Cell Therapy: Investigation into the use of stem cells for corneal regeneration and repair, exploring their potential in treating corneal dystrophies and degenerations.
Biomechanical Studies: Research on corneal biomechanics and understanding the structural changes associated with corneal dystrophies and degenerations to develop interventions that strengthen or modify corneal properties.
These advancements and ongoing research endeavors aim to improve early diagnosis, develop more effective treatments, and ultimately enhance the management and outcomes for individuals affected by corneal dystrophies and degenerations. Clinical trials, collaborations between researchers, and advancements in technology continue to drive progress in this field.
Summary
Corneal dystrophy and degeneration encompass inherited or acquired conditions affecting the cornea, leading to impaired vision and discomfort. Dystrophies involve genetic abnormalities causing material buildup, while degenerations result from various factors.
Diagnosis requires thorough eye exams, and treatment focuses on symptom management and preserving vision, with ongoing research aiming to develop advanced therapies for improved outcomes in these corneal conditions.