Barotrauma and volutrauma are two distinct but interconnected forms of lung injury often observed in patients receiving mechanical ventilation in intensive care settings. Barotrauma occurs when there’s excessive pressure applied to the lungs, leading to damage of the lung tissue, air leaks, and potentially pneumothorax (collapsed lung). This damage is primarily caused by high-pressure mechanical ventilation settings.
On the other hand, volutrauma results from over-distension of the alveoli due to large tidal volumes during ventilation, causing stress and injury to the lung tissue. Both barotrauma and volutrauma can contribute to a condition known as ventilator-induced lung injury (VILI), which can exacerbate respiratory distress in critically ill patients. Hence, managing ventilator settings and strategies to minimize these risks are crucial in preventing further lung damage in such cases.
What is Barotrauma?
Barotrauma refers to physical damage or injury caused to body tissues, particularly in the ears, sinuses, lungs, or other air-containing spaces due to changes in pressure. In the context of the respiratory system, barotrauma specifically pertains to lung injury resulting from exposure to excessive pressure.
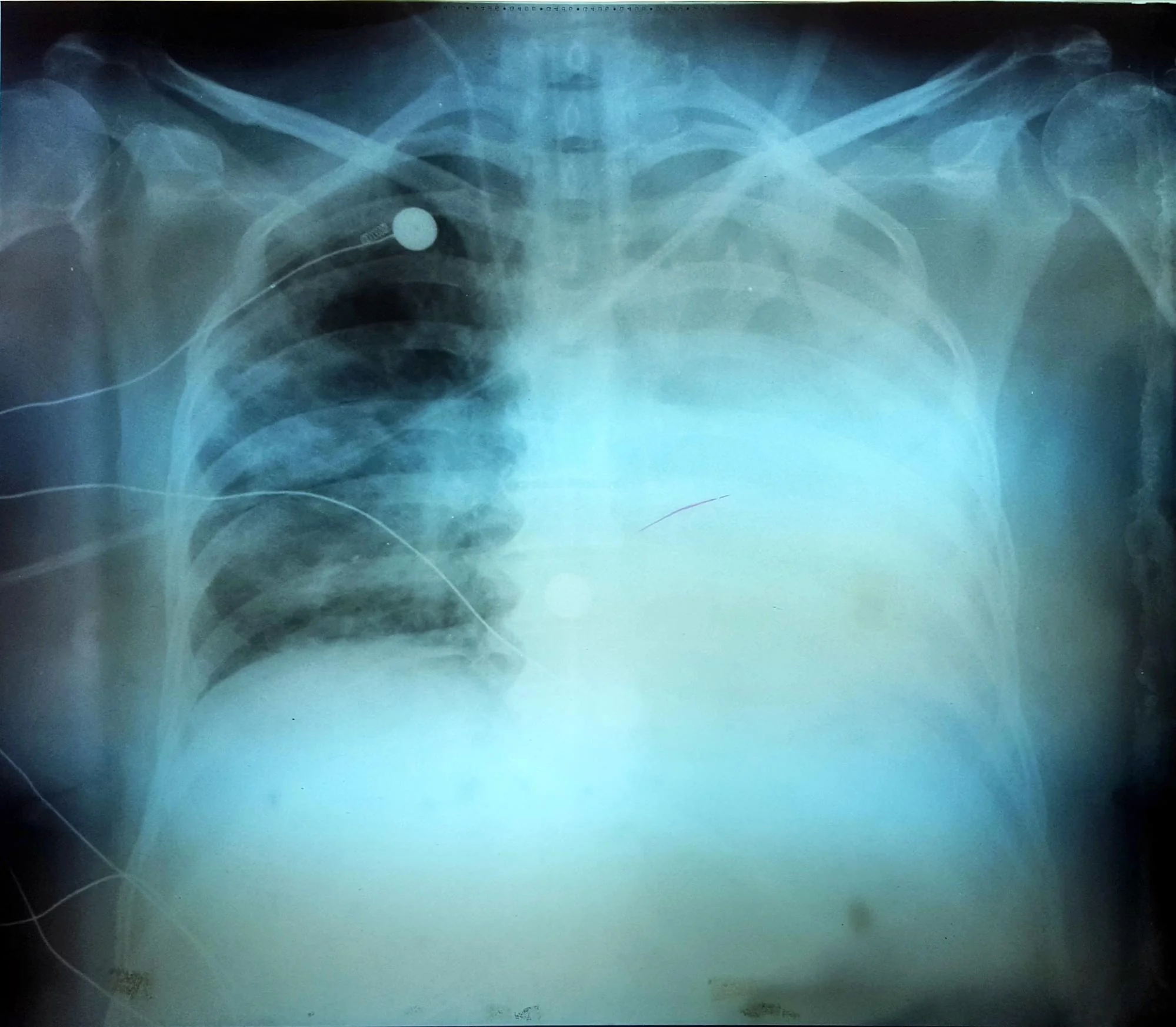
This condition commonly occurs in scenarios such as scuba diving, high-altitude environments, or medical settings like mechanical ventilation where the lungs are subjected to increased pressure levels beyond their tolerance, leading to tissue damage, air leaks, and potential complications like pneumothorax (collapsed lung) or pulmonary interstitial emphysema.
Symptoms of Barotrauma
Symptoms of barotrauma can vary depending on the affected area of the body. In the context of lung-related barotrauma, the symptoms may include:
- Chest pain
- Shortness of breath
- Difficulty breathing
- Rapid heart rate
- Coughing
- Feeling of pressure or tightness in the chest
- Bluish skin color (in severe cases)
- Pneumothorax (collapsed lung) symptoms: sudden sharp chest pain, difficulty breathing, and in severe cases, shock
Causes of Barotrauma
Barotrauma can be caused by various factors that result in rapid or extreme changes in pressure on body tissues. The primary causes include:
- Pressure Changes: Sudden or rapid changes in pressure, such as those experienced during scuba diving, flying in airplanes, or ascending/descending in elevators or mountainous areas, can affect air-containing spaces within the body.
- Mechanical Ventilation: In medical settings, particularly during mechanical ventilation in intensive care units, high-pressure settings or improper ventilation techniques can lead to excessive pressure on the lungs, causing barotrauma.
- Underwater Activities: Scuba diving or free diving where rapid changes in water pressure occur can affect the ears, sinuses, and lungs, leading to barotrauma in these areas.
- Explosive Blasts: Exposure to explosive blasts, such as those in combat zones or industrial accidents, can create sudden changes in atmospheric pressure, causing barotrauma injuries.
- Blocked Eustachian Tubes: In the case of ear barotrauma, blockages in the Eustachian tubes can prevent equalization of pressure between the middle ear and the environment during pressure changes, leading to injury.
- Altitude Changes: Rapid ascents or descents in altitude, especially in aviation, can cause barotrauma in the ears and sinuses due to the pressure changes.
What is Volutrauma?
Volutrauma refers to a type of lung injury that occurs due to excessive stretching or over-distension of the alveoli (small air sacs in the lungs) beyond their physiological limits. This condition arises when mechanical ventilation delivers tidal volumes (the amount of air entering and leaving the lungs during each breath) that are excessively high or when the respiratory rate is too rapid.
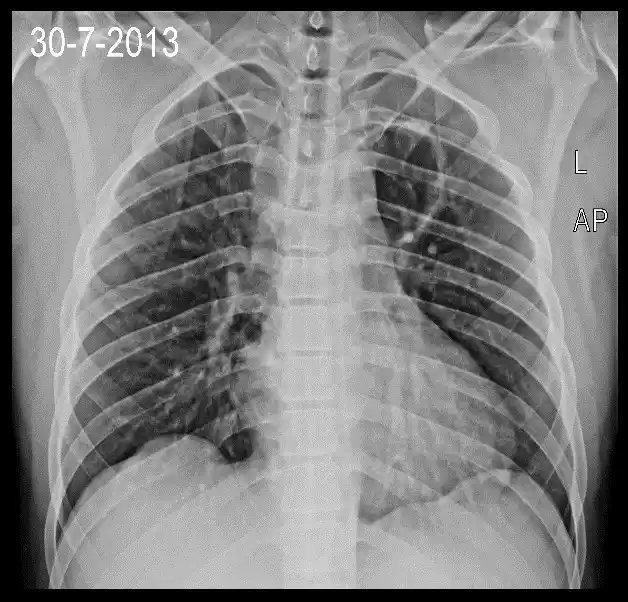
Prolonged exposure to high tidal volumes can cause damage to the delicate lung tissues, particularly the alveoli, leading to inflammation, increased permeability, and subsequent lung injury. Volutrauma is one component of ventilator-induced lung injury (VILI) and is often associated with other forms of ventilator-related damage such as barotrauma and atelectrauma.
Managing ventilator settings to prevent over-distension of the alveoli is crucial in minimizing the risk of volutrauma and improving patient outcomes during mechanical ventilation in critically ill individuals.
Symptoms of Volutrauma
Volutrauma primarily affects the lungs, and its symptoms may not be immediately apparent, but over time, they can manifest as:
- Worsening respiratory function: Increased difficulty in breathing or heightened respiratory distress.
- Hypoxemia: Reduced oxygen levels in the blood, leading to symptoms like confusion, rapid breathing, or bluish discoloration of the skin (cyanosis).
- Increased work of breathing: The patient may exhibit signs of increased effort in breathing, such as rapid or shallow breaths.
- Lung inflammation: Inflammatory responses within the lungs can contribute to symptoms like coughing or increased production of respiratory secretions.
- Chest discomfort or pain: Patients might experience chest tightness or discomfort due to the strain on the respiratory system.
- Decreased lung compliance: Reduced ability of the lungs to expand and contract properly, leading to decreased efficiency in breathing.
Causes of Volutrauma
Volutrauma typically arises due to mechanical ventilation practices that involve the delivery of excessive tidal volumes or pressures to the lungs. The primary causes include:
- High Tidal Volume: Ventilation strategies using tidal volumes that exceed the physiological capacity of the lungs can stretch and over-distend the alveoli, leading to volutrauma.
- Aggressive Ventilation: Ventilator settings that aim for rapid normalization of blood gases or aggressive correction of respiratory acidosis by using high tidal volumes may contribute to volutrauma.
- Inappropriate Ventilation Strategies: Ventilator settings that do not consider individual patient needs, such as inadequate adjustment for lung compliance or resistance, can lead to over-distension of alveoli.
- Prolonged Mechanical Ventilation: Continuous exposure to high tidal volumes over an extended period during mechanical ventilation can exacerbate lung injury, contributing to volutrauma.
- Failure to Adjust Ventilator Parameters: Lack of regular assessment and adjustment of ventilator settings based on the patient’s evolving respiratory status may result in volutrauma.
Comparison table of Barotrauma and Volutrauma
Here’s a comparison table outlining the key differences between Barotrauma and Volutrauma:
| Aspect | Barotrauma | Volutrauma |
| Definition | Lung injury due to excessive pressure | Lung injury due to over-distension of alveoli |
| Cause | Result of pressure changes | Caused by excessive tidal volumes in ventilation |
| Primary Effect | Tissue damage, air leaks, pneumothorax | Stretching and damage to alveoli |
| Common Scenarios | Scuba diving, flying, mechanical ventilation | Mechanical ventilation strategies |
| Affected Area | Lungs, ears, sinuses | Primarily affects lung tissue (alveoli) |
| Manifestation | Chest pain, difficulty breathing, coughing | Respiratory distress, hypoxemia, increased effort |
| Treatment Approach | Address pressure differentials, lung reinflation | Adjust ventilation settings, prevent over-distension |
| Prevention | Proper equalization, controlled pressure changes | Optimal ventilation strategies, monitoring |
Similarities between Barotrauma and Volutrauma
While Barotrauma and Volutrauma differ in their primary causes and affected areas, they do share some similarities:
- Lung Injury: Both Barotrauma and Volutrauma cause damage to lung tissues, albeit through different mechanisms. Barotrauma damages lung tissue due to excessive pressure, while Volutrauma results from over-distension of alveoli during mechanical ventilation.
- Respiratory Complications: Both conditions can lead to respiratory distress and compromised lung function. Barotrauma can cause symptoms like difficulty breathing and chest pain, while Volutrauma can result in increased work of breathing and decreased lung compliance.
- Ventilator-Associated Risk: Both Barotrauma and Volutrauma are associated with mechanical ventilation in medical settings. Barotrauma can occur due to high-pressure settings during ventilation, while Volutrauma is specifically linked to inappropriate ventilator strategies causing over-distension of alveoli.
- Potential Severity: In severe cases, both conditions can lead to significant complications. Barotrauma can result in pneumothorax (collapsed lung) and other serious issues, while Volutrauma contributes to ventilator-induced lung injury, which can exacerbate respiratory distress in critically ill patients.
Understanding these similarities is crucial in identifying and managing these conditions promptly, especially in medical settings where mechanical ventilation is utilized, to minimize the risk of lung damage and improve patient outcomes.
Treatment Options for Barotrauma and Volutrauma
Treatment approaches for Barotrauma and Volutrauma involve managing the underlying causes, alleviating symptoms, and preventing further damage.

Here are the general treatment options for each:
Barotrauma Treatment:
- Observation and Monitoring: Assess the severity of the condition and closely monitor the patient’s symptoms. Mild cases might resolve without specific interventions.
- Oxygen Therapy: Provide supplemental oxygen to improve oxygen levels in the blood and alleviate respiratory distress.
- Pain Management: Administer pain relief medications to alleviate chest pain or discomfort associated with Barotrauma.
- Drainage or Intervention: Severe cases, such as pneumothorax (collapsed lung), might require procedures like chest tube insertion to remove air or fluid from the pleural space.
- Preventive Measures: Educate individuals prone to Barotrauma (e.g., scuba divers, pilots) about equalization techniques to prevent future incidents.
Volutrauma Treatment:
- Ventilator Adjustment: Modify ventilator settings to ensure that tidal volumes and pressures delivered are within safe limits, preventing over-distension of the alveoli.
- Lung Protective Strategies: Implement lung-protective ventilation strategies, such as using lower tidal volumes and adjusting positive end-expiratory pressure (PEEP) to prevent further lung injury.
- Optimization of Ventilation: Regularly assess and adjust the ventilator settings based on the patient’s lung compliance, oxygenation, and respiratory status to minimize the risk of Volutrauma.
- Avoidance of Risk Factors: Minimize risk factors contributing to Volutrauma, such as prolonged high-pressure mechanical ventilation, by using appropriate ventilation strategies.
- Supportive Care: Provide supportive care to manage respiratory distress, oxygenation, and other associated complications. This may include supplemental oxygen, bronchodilators, or other supportive therapies.
Early recognition, prompt intervention, and appropriate management of the underlying conditions are essential. Healthcare professionals need to tailor treatment strategies based on the severity of the condition and the individual patient’s needs to prevent further lung damage and improve outcomes.
Effects of Barotrauma and Volutrauma on Different Organs
Barotrauma and Volutrauma primarily impact the respiratory system, particularly the lungs, but their effects can also extend to other organs in the body:
Barotrauma Effects:
- Lungs: Barotrauma primarily affects the lungs, causing damage to lung tissue, air leaks, and potential complications like pneumothorax (collapsed lung) or pulmonary interstitial emphysema.
- Ears and Sinuses: Barotrauma during pressure changes (e.g., scuba diving, flying) can lead to injuries in the ears and sinuses, resulting in pain, ear fullness, or sinus discomfort.
- Cardiovascular System: Severe Barotrauma, especially if it leads to significant respiratory compromise, can affect the cardiovascular system by impacting oxygenation levels and increasing stress on the heart.
Volutrauma Effects:
- Lungs: Volutrauma primarily affects the lung tissue, specifically the alveoli. Over-distension of alveoli can lead to lung inflammation, decreased lung compliance, and contribute to ventilator-induced lung injury.
- Respiratory System: It can exacerbate respiratory distress, leading to increased work of breathing, decreased efficiency in gas exchange, and compromised oxygenation.
- Systemic Effects: Severe Volutrauma and subsequent ventilator-induced lung injury can trigger systemic inflammatory responses, potentially affecting other organs and systems in the body.
While the direct impact of Barotrauma and Volutrauma is primarily on the respiratory system, severe cases or complications can influence overall physiological functions, including cardiovascular stability and systemic inflammation. Managing these conditions promptly and effectively is crucial to minimize their adverse effects on multiple organ systems and to improve patient outcomes.
Prevention Strategies
Prevention strategies for Barotrauma and Volutrauma involve various measures to reduce the risk of lung injuries due to pressure changes or mechanical ventilation.
Here are some preventive measures for each:
Barotrauma Prevention:
- Equalization Techniques: Educate individuals involved in activities such as scuba diving or flying about proper equalization techniques to prevent pressure-related injuries in the ears and sinuses.
- Pressure Management: Encourage gradual pressure changes during altitude changes in airplanes or mountainous regions to allow the body to adapt gradually.
- Monitoring and Safety: Maintain proper equipment, adhere to safety protocols, and ensure regular checks of scuba diving equipment to prevent pressure-related accidents.
- Avoidance of Rapid Pressure Changes: Minimize rapid changes in pressure, especially in situations where individuals are prone to Barotrauma, to reduce the risk of ear, sinus, or lung injuries.
Volutrauma Prevention:
- Lung Protective Ventilation: Utilize lung-protective ventilation strategies in critically ill patients requiring mechanical ventilation, such as using lower tidal volumes and adjusting positive end-expiratory pressure (PEEP).
- Ventilator Management: Regularly assess and adjust ventilator settings based on the patient’s lung compliance, respiratory status, and oxygenation needs to prevent over-distension of the alveoli.
- Careful Monitoring: Monitor patients on mechanical ventilation closely to identify signs of over-distension or ventilator-induced lung injury promptly.
- Individualized Approach: Tailor ventilation strategies to individual patient needs, considering factors like lung compliance, resistance, and underlying lung conditions.
- Staff Education and Training: Ensure healthcare professionals are well-trained in appropriate ventilation strategies and are aware of the risks associated with high tidal volumes or pressures during mechanical ventilation.
By implementing these preventive strategies, it is possible to minimize the risk of Barotrauma and Volutrauma in various settings, whether related to pressure changes in recreational activities or mechanical ventilation in medical settings, ultimately reducing the occurrence and severity of associated lung injuries.
Impact of Barotrauma and Volutrauma on Health
Barotrauma and Volutrauma can have significant impacts on health, primarily affecting the respiratory system, but their repercussions can extend beyond the lungs:
Impact of Barotrauma:
- Respiratory Complications: Barotrauma can lead to severe respiratory distress, chest pain, difficulty breathing, and coughing. In severe cases, it can result in pneumothorax (collapsed lung) or pulmonary interstitial emphysema.
- Ear and Sinus Issues: Pressure-related injuries during activities like scuba diving or flying can cause ear pain, hearing loss, ear fullness, sinus discomfort, and other related symptoms.
- Cardiovascular Effects: Severe Barotrauma compromising oxygenation can strain the cardiovascular system, impacting heart function and overall cardiovascular stability.
Impact of Volutrauma:
- Lung Injury: Volutrauma primarily affects the lungs by causing damage to the delicate alveoli, leading to lung inflammation, decreased compliance, and ventilator-induced lung injury.
- Respiratory Distress: It can exacerbate respiratory distress, increase work of breathing, and compromise gas exchange, leading to hypoxemia and potential respiratory failure.
- Systemic Effects: Severe cases of Volutrauma can trigger systemic inflammatory responses, affecting multiple organ systems and potentially contributing to further complications.
Barotrauma and Volutrauma can have serious repercussions on health when left untreated, including respiratory impairment, cardiovascular strain and potential systemic complications due to inflammation or compromised gas exchange. Therefore, proper management plans, prompt interventions and preventive steps must be put in place in order to minimise their negative impacts and ensure better outcomes for those affected by these illnesses.
Conclusion
Barotrauma and Volutrauma represent distinct yet impactful lung injuries. Barotrauma results from pressure changes, causing tissue damage primarily in the lungs, ears, or sinuses. In contrast, Volutrauma occurs during mechanical ventilation, overstressing lung alveoli. Both conditions jeopardize respiratory function, causing distress, lung damage, and potential systemic repercussions. Prompt recognition, preventive measures, and tailored interventions are essential to mitigate these injuries, improving patient outcomes in diverse settings.