Parkinsons and Huntingtons Disease are both neurological diseases that cause severe pain However, they differ in their root causes as well as their symptoms and progress. Understanding the difference is vital for identifying the condition early, and providing effective treatment, and assistance to families and individuals affected by these disorders.
We will look at the key differences between Huntington’s disease and Parkinson’s by shedding light on their distinctive characteristics as well as the challenges they pose for the people who suffer from them.
Explanation of Parkinson’s Disease
Parkinsons disease, also known as PD is a long-lasting and progressive neurological condition that mostly affects the control of movement. It is characterized by the degeneration of specific brain cells, notably dopamine-producing neurons located in a part of the brain known as the substantia nerve. Dopamine can be described as a neurotransmitter that is responsible for transmitting signals to control the coordination and movement of muscles.
As dopamine-producing neuronal functions decline people with Parkinson’s disease suffer from a wide range of motor symptoms. These include stiffness, tremors bradykinesia (slowness of movement), and postural instability. These signs tend to increase in severity as time passes, affecting the ability of a person to complete daily tasks and preserve their health.
Parkinson’s disease may also cause non-motor symptoms, like mood disorders, cognitive changes, and autonomic dysfunction which may further aggravate the disease. Although there is no treatment for the disease, a variety of methods of treatment, including medication or physical therapy, as well as surgical interventions, can assist in alleviating symptoms and enhance the general health of those affected by the condition. Early diagnosis and proper management are essential to improve the quality of life for people suffering from Parkinson’s disease.
Explanation of Huntington’s Disease
Huntington’s disease, also known as HD is a hereditary, progressive neurological disorder that leads to the destruction of specific neurons within the brain. The disease is an autosomal-dominant genetic disease which means that a person only requires one copy of the gene that is defective (HTT gene) from both parents to be affected.
The main characteristic of Huntington’s illness is the progressive and constant decline in motor and cognitive control. People with Huntington’s disease generally suffer from a variety of symptoms, such as:
- Uncontrollable, involuntary motions (chorea)
- Cognitive impairment, which includes memory issues and difficulties in reasoning and decision-making
- Disorders of mood, like depression, anxiety, or anger
- Behavior changes, including the tendency to be impulsive and withdraw from social situations
- Decrease in functional capabilities that affect daily living
The first signs of Huntington’s disease typically occur in the latter part of adulthood generally between the age of 30 and 50 but it can be seen at any time. The course of progression differs from person to but generally results in significant disability and a diminished quality of life with time.
Huntington’s disease is caused due to a change in the HTT gene, which results in the creation of abnormal forms of a protein known as huntingtin. The growth of these proteins that are abnormal in the brain cells is a factor in the neurodegenerative nature of the disease.
There is currently an effective treatment for the disease Huntington’s but a range of treatments, which include medication and supportive care can ease the symptoms and enhance living quality of patients.
Genetic testing and counseling are vital for people who have a family history of Huntington’s disease in order to comprehend their risks and make informed choices about healthcare and family planning.
Comparison Table of Parkinson’s and Huntington’s Disease
Here’s a comparison table highlighting the key differences between Parkinson’s disease and Huntington’s disease:
| Aspect | Parkinson’s Disease | Huntington’s Disease |
|---|---|---|
| Nature of Disorder | The neurodegenerative disorder primarily affects movement. | A neurodegenerative disorder affects both movement and cognition. |
| Onset | Typically occurs in later adulthood, usually after age 60. | Usually starts in adulthood, typically between ages 30 and 50. |
| Genetic Inheritance | Generally not inherited; most cases are sporadic. | Autosomal dominant inheritance with a known genetic mutation (HTT gene). |
| Genetic Mutation | No specific gene mutation is associated with Parkinson’s. | Mutation in the HTT gene leads to the production of abnormal huntingtin protein. |
| Motor Symptoms | Tremors, bradykinesia (slowness of movement), rigidity, postural instability. | Involuntary movements (chorea), muscle rigidity, bradykinesia, and dystonia. |
| Cognitive Symptoms | Mild cognitive impairment can occur in later stages. | Prominent cognitive decline, including memory loss, decision-making problems, and mood changes. |
| Mood and Behavior | Mood disturbances (depression, anxiety) may occur. | Mood disturbances (irritability, impulsivity) and behavioral changes are common. |
| Neurotransmitter | Dopamine deficiency in the brain. | Complex alterations in neurotransmitters, including dopamine. |
| Diagnosis | Based on clinical symptoms and may involve brain imaging (e.g., MRI or PET scans). | Genetic testing confirms the presence of the HTT gene mutation. |
| Treatment | Medications (e.g., levodopa), physical therapy, and deep brain stimulation. | Symptom management with medications (e.g., antipsychotics), psychotherapy, and supportive care. |
| Progression | Gradual progression with variable rates of decline. | Progressive and relentlessly deteriorating, leading to significant disability. |
| Life Expectancy | Typically, individuals live for many years after diagnosis. | Life expectancy is reduced, usually 15-20 years after onset. |
It’s important to note that while this table highlights the primary differences between the two diseases, both Parkinson’s and Huntington’s diseases are complex conditions with varying presentations and individual experiences. Management and care for these diseases are tailored to each patient’s specific needs.
Importance of understanding the differences
Understanding the distinctions between Huntington’s and Parkinson’s disease is vital for a variety of reasons:
- Accurate Diagnosis: Understanding the differences between these conditions assists healthcare professionals in making precise diagnoses. A timely and accurate diagnosis is essential to provide proper treatment and support for patients.
- Tailored Treatment: Different illnesses require different approaches to treatment. Knowing the difference allows medical professionals to create customized treatment plans that address the distinct problems and symptoms that are related to each illness.
- Medication Management: A variety of drugs employed to treat these illnesses have different mechanisms of action as well as potential negative side consequences. Knowing these differences enables medical professionals to prescribe the most appropriate medications while minimizing negative side effects.
- Genetic Counseling: Huntington’s disease is an obvious genetic component as is genetic counseling crucial for those who are at risk of developing it. Knowing the genetic cause of the disease allows individuals to make informed choices regarding testing for genetics and planning for families.
- Support and Care: Support networks and caregivers play an important role in the lives of those suffering from these conditions. Knowing what makes them different enables caregivers to give more efficient care and assistance that is tailored to the requirements of the loved family members.
- Researchers and Development: Researchers who study Huntington’s disease and Parkinson’s disease require an understanding of all distinctions to determine possible therapeutic targets and to develop more efficient treatments.
- Public Health: Public awareness campaigns and educational programs can gain from accurate and up-to-date information regarding diseases. A better understanding of the disease reduces stigma and can increase compassion and understanding for the affected person as well as their family members.
- Advocacy and Funding: The advocacy efforts that are used to raise money for the research of and provide support for these conditions are more successful when the public as well as policymakers and philanthropic organisations are aware of the unique challenges presented by Huntington’s and Parkinson’s diseases.
- Qualitative of Life: Knowing the distinctions between these diseases enables patients and their families with the ability to better manage their condition make educated decisions and implement strategies to enhance their quality.
- Ethical Considerations: Understanding the differences in HTML0 poses ethical issues in concerns such as the genetic test, reproductive options, and care for the end of life. Discussions on ethics benefit from accurate details about the illnesses.
Understanding the distinctions between Huntington’s disease and Parkinson’s disease is vital to improving diagnosis, treatment, and support for people who are affected by these diseases. This also aids in research as well as advocacy and public education efforts that aim to improve the quality of life for those with these neurodegenerative diseases.
Specific motor symptoms of Parkinson’s disease
A few of the motor symptoms that are associated with Parkinson’s disease are:
- Tremors: The shaking or tremors of fingers, hands, or any other body part in particular at rest is the most well-known symptom of Parkinson’s disease. They are usually called “resting tremors.”
- Bradykinesia: Bradykinesia refers the slower movement. People suffering from Parkinson’s disease might be unable to initiate and execute actions, which can make simple tasks such as getting up from a chair or walking more difficult.
- Muscle Rigidity: Stiffness in the muscles can be a frequent sign of Parkinson’s illness. It can affect different muscle groups, resulting in less flexibility and reduced mobility. The pain of rigidity can be intense and can make movements less fluid.
- Postural Instability: Balance issues and the tendency to lean or fall backward are common in later phases of disease Parkinson’s. This makes it more difficult to keep an upright posture. It can also increase the risk of falling.
- Akinesia: Refers to the loss of muscle movements that are voluntary, which results in temporary paralysis and “freezing.” This is often the case at the beginning of gait which makes it hard to begin walking.
- Dystonia Dystonia is a condition that causes involuntary muscular contractions which cause repetitive or twisting movements. It can also cause abnormal postures or prolonged muscle contractions. It can affect different body parts, like fingers, the toes, or the neck.
- Micrographia: It is possible for Parkinson’s illness to alter the handwriting of a patient resulting in smaller and constricted or difficult-to-read writing. This is called micrographia.
- “Masklike-Face”: An inability to express facial expressions properly is common among people with Parkinson’s disease. It gives the face the appearance of a “mask-like” appearance. The reason for this is the stiffness and rigidity of the muscles.
- Reduced arm swing: A reduced natural arm swing when walking is a typical symptom that is characteristic of Parkinson’s Disease. The arms tend to remain closer to the person.
- Speech and swallowing Problems: Many individuals with Parkinson’s disease experience changes in their speech patterns and voice such as soft speech and monotone or slurred speech. Problems swallowing (dysphagia) may also be present.
It’s crucial to recognize that the severity and frequency of these symptoms may differ from one person to the next. Furthermore, non-motor manifestations such as cognitive issues, mood disorders, and autonomic dysfunction may also be part of the general manifestation that is characteristic of Parkinson’s illness.
Early diagnosis and correct treatment can help people suffering from Parkinson’s disease to manage these motor issues and preserve their level of living.
Cognitive and psychiatric symptoms of Parkinson’s
Parkinson’s disease may also cause an array of mental and psychiatric symptoms. These non-motor afflictions can dramatically affect well-being and are essential to take into consideration when managing the disease.
A few of the psychiatric and cognitive symptoms that are associated with Parkinson’s disease are:
Cognitive Impairment:
- Mild Cognitive Impairment (MCI): Many sufferers of Parkinson’s disease have minor cognitive impairments like difficulties in attention, memory, and executive functions. These changes might not hinder greatly daily activities, but they may be apparent.
- Dementia: In some cases, cognitive impairment may progress into more serious forms of dementia, referred to as Parkinson’s Disease (PDD). Signs and symptoms of PDD may include memory impairments in the form of confusion, confusion, impaired judgment, and difficulty in acquiring visual and language skills.
Psychiatric Symptoms:
- Depression: Depression happens to be one of the frequently reported symptoms of psychiatric illness in Parkinson’s disease. It may manifest as constant sadness, a loss of interest in previously enjoyable activities, a change of appetite and sleep issues, and feelings of despair.
- Anxiety: The anxiety disorders which include generalized anxiety disorder as well as social anxiety are most common in people suffering from Parkinson’s disease. Anxiety may manifest as a lot of anxiety, restlessness, and physical symptoms such as trembling and sweating.
- Apathy: It refers to an absence of interest or motivation in the activities. It is different from depression and characterized by decreased energy and an inability to express emotions.
- Psychosis: Certain people with Parkinson’s illness might suffer from psychotic symptoms, including hallucinations (seeing or hearing things that don’t exist) as well as the occurrence of delusions (false belief systems). These signs are more frequent when the disease is in its advanced stage of disease and could be connected with side effects from medication.
- Impulse Control Disorders (ICDs): ICDs are defined by the inability to resist impulses or urges, which can result in actions that could be dangerous or even disruptive. Common ICDs that are associated with Parkinson’s disease include hypersexuality, compulsive gambling, and eating disorders that are characterized by binge eating.
- Sleep Disorders: Sleep problems are typical in Parkinson’s disease. They could include restless legs, insomnia syndrome along rapid eye movements (REM) sleep disorder, in which people physically perform their dream scenes in sleep.
- Fatigue: A lot of people suffering from Parkinson’s disease experience extreme fatigue that can be both mental and physical in the way that it manifests.
It’s crucial to understand that not all people with Parkinson’s disease experience the psychiatric or cognitive symptoms. The severity and the time at which they begin will vary. Early recognition and treatment of these symptoms are crucial for enhancing the quality of life for those suffering from Parkinson’s disease.
Treatment options include medication and psychotherapy, lifestyle adjustments as well and adjustments to medications for Parkinson’s disease to treat particular symptoms. The support of family and caregivers is essential in addressing the non-motor components of the condition.
Medications for Parkinson’s disease
The treatment for Parkinson’s disease usually is a mixture of medicines that are designed to ease motor and, in a few instances some cases, non-motor symptoms. Parkinson’s medications primarily function by either boosting dopamine levels within the brain or altering other neurotransmitters to enhance motor control.
Here are a few of the most commonly prescribed drugs to treat Parkinson’s disease:
- Carbidopa/Levodopa (Sinemet): This combination medication is among the most efficient treatment options for Parkinson’s condition. Levodopa converts into dopamine within the brain, while carbidopa keeps levodopa from getting broken down too quickly into the bloodstream. This combo helps to boost dopamine levels and helps improve motor symptoms.
- Dopamine Agonists: These medications mimic the actions of dopamine in the brain. They are effective either on their own or together with levodopa. Dopamine agonists that are commonly used include pramipexole (Mirapex) Ropinirole (Requip) and the rotigotine (Neupro).
- MAO-B Inhibitors: Monoamine oxidase B (MAO-B) inhibitors such as rasagiline (Azilect) and selegiline (Eldepryl) block Dopamine’s breakdown within the brain, thereby helping to increase its supply.
- COMT Inhibitors: Catechol-O-methyltransferase (COMT) inhibitors, like entacapone (Comtan) and tolcapone (Tasmar), prolong the effects of levodopa by preventing its breakdown in the peripheral nervous system.
- Anticholinergic Medicines: These medications, such as trihexyphenidyl (Artane) or benztropine (Cogentin) are able to reduce muscle stiffness and tremors by cutting down the acetylcholine activity, another neurotransmitter.
- Amantadine (Symmetrel): Amantadine can offer alleviation in dyskinesias (involuntary movements) and can help alleviate motor symptoms. It is a drug that can be used by itself or in conjunction with other medicines.
- Adenosine A2A receptor antagonists Such drugs as istradefylline (Nourianz) can be utilized to decrease off-time (periods when medication isn’t working efficiently) for patients who experience changes in their response to levodopa.
- NMDA receptor antagonists: Memantine, a medication (Namenda) can be utilized to treat cognitive impairment and other non-motor symptoms of Parkinson’s disease.
It is important to remember that the treatment for patients with Parkinson’s disease is incredibly individual. A neurologist or a specialist in movement disorders usually evaluates the patient’s symptoms, their responses to medicines, and any other side effects to formulate an individual treatment strategy.
The aim is to attain the best level of control for symptoms while minimizing the risk of side effects and altering medications as the condition progresses.
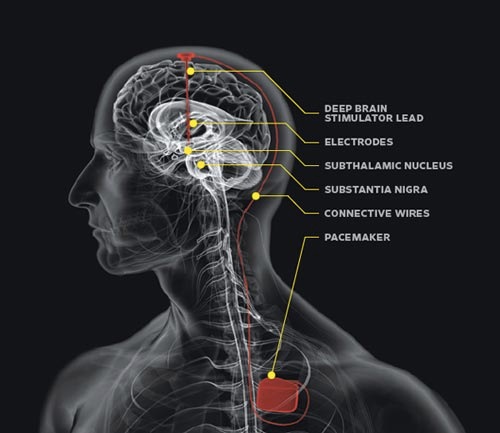
In the more severe cases of Parkinson’s disease, where medication alone fails to be efficient, surgical treatments such as the stimulation of deep in the brain (DBS) could be considered. DBS involves implanting electrodes into certain brain regions to regulate neural activity and ease symptoms.
As with all medical conditions, it is essential for those who suffer from Parkinson’s disease to work closely with their healthcare providers to track their symptoms, alter medications as necessary, and receive the best care that addresses both motor as well as non-motor aspects of the disease.
Surgical interventions for Parkinson’s disease
The possibility of surgical intervention is considered for patients suffering from Parkinson’s disease, when medication is no longer efficient in reducing their motor symptoms, or when medications-related side effects start to become problematic. The surgical procedures are designed to control irregular brain function and increase motor performance.
Here are a few of the principal surgical treatments used to treat Parkinson’s disease:
- Deep Brain Stimulation (DBS): DBS is among the most commonly used and efficient surgical treatments for Parkinson’s disease. It involves the placement of electrodes with thin wires in specific brain regions, usually that of the subthalamic nucleus (STN) or the globus pallidus intermedia (GPi) as well as the thalamus. These electrodes are connected to neurostimulator devices (similar to pacemakers) typically placed beneath the chest skin or the abdomen. The neurostimulator transmits electrical impulses through the brain to help which are used for modulating abnormal neural activity and decreasing motor symptoms.
The benefits of DBS include better motor function, less the tremors of tremors, fewer dyskinesias (involuntary movements), and the capacity to decrease dosages of medications and reduce the risk of adverse reactions.
- Focused Ultrasound ablation (FUS): Focused ultrasound ablation is a non-invasive surgical procedure that utilizes high-intensity ultrasound waves in order to destroy and target particular brain tissues which is the cause of Parkinson’s disease. It is generally used to treat those who are not responding well to drugs but aren’t suitable for conventional DBS procedures.
FUS is a method to focus on either the globus pallidus (GPi) as well as the subthalamic nuclear nucleus (STN). This procedure has similar advantages as DBS however without the requirement to implant electrodes.
- Lesions Procedures The past procedures for lesioning required surgically creating small lesions (damaged regions) in particular brain regions that are responsible for Parkinson ‘s-related symptoms. However, the procedures are becoming rare because of having access to DBS as well as FUS. They are only used in cases when DBS or FUS are not appropriate.
- Pallidotomy: The procedure involves making a lesion within the pallidum globus (GP) to alleviate dyskinesias as well as other motor symptoms.
- Thalamotomy: Thalamotomy causes lesions in the thalamus that help ease tremors, in particular instances where they are the primary symptoms.
It’s crucial to understand that not all patients who suffer from Parkinson’s disease are suitable for surgery and the choice to undergo surgery is taken after an extensive examination by a neurologist or specialist in movement disorders.
The selection of a surgical procedure is based on a variety of aspects, such as the patient’s health status, age, overall health, specific symptoms, and treatment goals for each individual.
The use of surgical procedures can provide substantial relief from motor-related symptoms and enhance the quality of life of people suffering from Parkinson’s disease. However, they have potential risks that require extremely careful after-operative treatment and follow-up care to maximize their effects.
Potential breakthroughs and emerging treatments
In my last information report in the month of September 2021, there were a number of interesting research areas and possible breakthroughs in the area that dealt with Parkinson’s disease. Although I am unable to provide any information about developments after the date of my last update, I will provide a brief overview of some promising directions and treatment options being studied:
- Disease-Modifying Therapies: Researchers were currently researching therapies that could slow or stop the progress of Parkinson’s. These included medications and treatments that were designed to safeguard and rejuvenate dopamine-producing brain neurons.
- Gene Therapy: Gene therapies were being studied as a possible solution to tackle the molecular and genetic causes that contribute to the development of Parkinson’s. The therapies were designed to release beneficial genes to the brain in order to restore normal function.
- Immunotherapies: The use of immunotherapies such as vaccines or antigens that target alpha-synuclein (a protein that is associated with Parkinson’s disease) is in the process of development to help reduce the amount and accumulation of harmful protein aggregates within the brain.
- Therapy with Stem Cells: The study of stem cells showed promise in the creation of dopamine-producing cells that could be transplanted into the brains of people suffering from Parkinson’s disease in order to replace the ones that are lost because of the disease. Clinical trials are ongoing to test the efficacy and safety of these therapies.
- Focused Ultrasound and other non-invasive approaches: Advancements in non-invasive methods such as focused ultrasound and transcranial magnetic stimulation have been studied as possible treatments to alleviate motor symptoms and enhance general brain function.
- Precision Medicine: Advances in genomics and personalized medicine have led to more individualized treatments based on a person’s genetic profile, which enables more precise and efficient treatments.
- The Internet of Health and Wearable Devices: The use of wearable devices and digital health technology was increasing, bringing new methods to manage and monitor Parkinson’s symptoms. These devices aim to enhance care and offer prompt intervention when it is necessary.
- Neuroprotection Strategies: Researchers are studying a variety of chemicals and strategies for protecting neurons and decreasing neuroinflammation as a way of maintaining the brain’s function in people suffering from Parkinson’s disease.
- Telemedicine as well as Remote Monitoring: Remote monitoring and telemedicine solutions have become more crucial, especially in the wake of the COVID-19 pandemic, which allows for ongoing monitoring and care of Parkinson’s patients.
It’s crucial to be aware that research into Parkinson’s disease is in progress as new discoveries and novel treatments may have emerged since my last update of knowledge.
Anyone who is interested in the most recent advances in Parkinson’s disease research should seek out reliable sources like scientific journals, clinical trial registries, and trusted organizations focusing on Parkinson’s research as well as advocacy.
Also discussing treatment choices and participating in clinical trial trials with your healthcare doctor or specialist is vital to stay informed of the current advancements in the management of Parkinson’s disease.
Reference Books
Certainly! Here are some reference books on Parkinson’s disease that provide valuable information for both patients and healthcare professionals. Please note that the publication dates may vary, so it’s a good idea to check for the most recent editions for the latest information:
- “Parkinson’s Disease: Diagnosis and Clinical Management” by Stewart A. Factor and William J. Weiner
- This comprehensive book offers insights into the diagnosis and clinical management of Parkinson’s disease, including the latest treatments and research findings.
- “Parkinson’s Disease: Non-Motor and Non-Dopaminergic Features” edited by Oksana Suchowersky, Anthony E. Lang, and Daniel Tarsy
- Focuses on non-motor and non-dopaminergic aspects of Parkinson’s disease, exploring various symptoms and their management.
- “Parkinson’s Disease and Movement Disorders” edited by Joseph Jankovic and Eduardo Tolosa
- A comprehensive resource covering not only Parkinson’s disease but also other movement disorders, offering insights into diagnosis and management.
- “Parkinson’s Disease: Molecular Mechanisms Underlying Pathology” edited by Christian Wider and Serge Przedborski
- Provides a detailed look at the molecular mechanisms underlying Parkinson’s disease, which is valuable for researchers and clinicians.
- “Living Well with Parkinson’s Disease: What Your Doctor Doesn’t Tell You…That You Need to Know” by Gretchen Garie and Michael J. Church
- A practical guide for individuals and caregivers, offering advice on living a fulfilling life while managing Parkinson’s disease.
Conclusion
It is a nebulous neurological disorder that affects millions across the globe. While there isn’t a cure, the ongoing research and new treatments provide an opportunity to improve management and living quality.
Knowing the causes of Parkinson’s symptoms of the disease, both motor and non-motor and staying up-to-date on the latest developments will empower patients as well as healthcare professionals to tackle the difficulties associated with Parkinson’s disease successfully.
Through continued support in research, advocacy, and education advances are being made in pursuit of more effective treatments and, ultimately, a cure for this disease.